Background
Plasmablastic Lymphoma (PBL) is a neoplasm first described in 1997. On the original report, all the 16 patients had involvement of the oral cavity. However, more recent studies have identified PBL in a variety of anatomic locations. The diagnosis can be difficult because of the lack of expression of usual markers and overlapping features of B-cell lymphoma and plasma-cell neoplasm. Given its rarity and high fatality, there is no prospective studies and, consequently, there is no standard of care established for PBL.
Methods
This was a retrospective observational study carried out at a community cancer center. We reviewed the chart of all 458 patients diagnosed with Lymphoma in our service from December 2006 to December 2016 and included patients diagnosed with PBL during this period. Patients' electronic medical charts were reviewed for detailed information regarding demographics, treatment given and response to treatment as well as complications and outcome. Diagnosis of PBL was established by histopathologic examination and immunohistochemistry studies.
Results
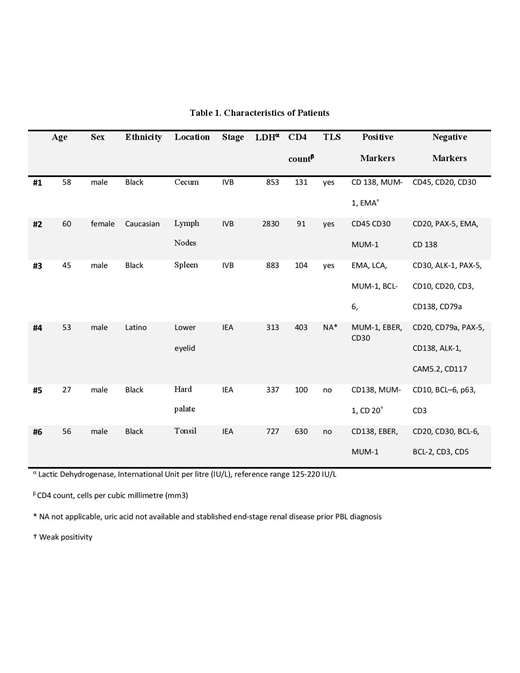
We found on our records six patients with diagnosis of PBL (Table 1), three of them presented initially without oral involvement and with Tumor Lysis Syndrome (TLS). We reviewed in detail three cases of PBL with dramatic outcome and this common feature of TLS. They were all managed appropriately with rasburicase, since this drug became broadly available after its FDA approval in 2009. Two cases were spontaneous TLS and one patient with PBL in the spleen developed TLS after high-dose steroids. All three patients died before any chemotherapy regimen could be administered.
All the patients in this study were HIV-positive, only four patients had CD4 count below 200/mm3. For one patient, there was not enough data available to assess for TLS.
Discussion
Despite comparative studies could not demonstrate an association between HIV status and outcome in PBL, a single center study showed exceptionally good outcome in HIV-positive patients with CD4 count above 200/mm3. Another study with immunosuppressed HIV-negative patients suggests poor outcome within this scenario. Interestingly, the patients with TLS in our study had CD4 count below 200/mm3, suggesting that immunosuppression may be associated with more aggressive disease and worse prognosis. In addition, the patients with TLS in our study didn't have involvement of the oral cavity, it remains unclear if extra-oral PBL correlates with unfavorable outcome.
Not only diagnosing but treating PBL poses an enormous challenge for oncologists since there is no standard of care established in treating this rare Lymphoma. At the moment of this publication, no prospective studies have been conducted and there is no publication describing spontaneous TLS in PBL. This short series of cases demonstrates a high prevalence of TLS (at least 50%), this may be an important feature to be considered in future studies. Furthermore, our report may raise awareness about the potentially poor outcome within this scenario. When diagnosis of PBL is suspected, screening for TLS should not be delayed and early aggressive management warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal