Introduction: Whether sickle cell disease (SCD) or its primary treatment, hydroxyurea (HU), limits reproductive potential in affected women is unknown. Females are born with a finite number of eggs. Anti-Mullerian Hormone (AMH), produced by immature ovarian follicles, is an established method to measure ovarian reserve. Two studies of AMH, one in adolescents with SCD and another in adult women with SCD exist, but neither normal AMH values nor the effect of HU on AMH are established in girls and women with SCD. The purpose of this study is to evaluate AMH levels in women who participated in the seminal study that led to FDA-approval for HU in adults with SCD, the Multi-Center Study of Hydroxyurea (MSH).
Methods: The MSH was a randomized placebo-controlled trial (RCT) of HU. The RCT demonstrated HU's efficacy, so a 10-year MSH extension study was conducted to assess HU's potential for "mutagenesis, teratogenesis and oncogenesis". Although no samples from the RCT remain, serum samples (n=285) were available for many women in the follow-up study (n=93). We measured AMH in these samples using the CLIA-certified electrochemiluminescence assay in clinical use at our institution (Esoterix Labs, Calabasas Hills, CA). The assay's reference median AMH in women ages 26 - 30 years is 4.20 ng/mL, and in women 36 - 40 years is 1.69 ng/mL. The assay's lower limit of detection is 0.015ng/mL. Samples with AMH levels beneath the detection limit were run in duplicate when sufficient sample existed; this did not change any results.
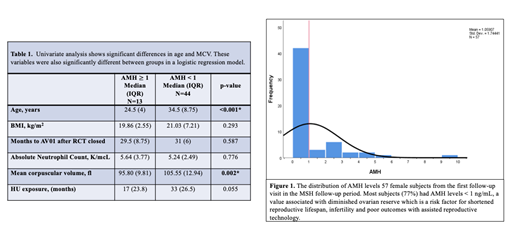
Here, we report AMH levels in female subjects (n=57) with a serum sample from the first annual follow-up visit (AV01). Descriptive statistics with median values reported for non-parametric variables (Mann Whitney U Test) were performed. AMH < 1 is associated with diminished ovarian reserve, a risk factor for shortened reproductive lifespan, infertility and poor outcomes with assisted reproductive technology. Therefore, we categorized AMH as normal (>/= 1 ng/ml) and low (<1 ng/ml). We initially evaluated factors associated with low AMH using the chi-squared and Mann Whitney U test for categorical and continuous variables, respectively. We then performed logistic regression analysis to evaluate the independent association of age, BMI, absolute neutrophil count (ANC), mean corpuscular volume (MCV) and months of HU exposure with AMH levels.
Results: Samples from the first post-study visit were available for 57 women; the median time to first post-study visit was 31 months (IQR 6.5) after RCT closure. Median values for the cohort were: AMH, 0.306ng/ml (IQR 1.162), age, 32.50 years (IQR 11), MCV, 102.0 fl (IQR 15.8), and HU exposure, 23.92 months (IQR 30.72). Figure 1 shows AMH distribution in the cohort. AMH levels were low in 77% (44 of 57) of the cohort. Table 1 compares patient characteristics of subjects with low AMH (n=44) versus normal AMH (n=13). In univariate analysis, subjects with low AMH were older (34.5 vs 24.5, p<0.001) and had larger MCV (105.55 vs 95.80, p=0.002). Median HU exposure time did not reach significance between low and normal AMH groups (33 months vs 17 months, p=0.055). In a logistic regression model, age [OR 1.252, (95% CI 1.066, 1.014), p=0.006] and MCV [OR 1.139, (95% CI 1.014, 1.279), p=0.028] were associated with low AMH while duration of exposure to HU [OR 1.01 (95% CI 0.91, 1.09), p=0.364], body mass index [OR 1.07 (95% CI 0.91, 1.25), P=0.442] and ANC [OR 1.39 (95% CI 0.91, 2.13), p=0.127) were not associated with low AMH.
Conclusions: Most women (77%) in this cohort had low AMH, associated with older age and higher MCV. This preliminary analysis raises concerns about diminished ovarian reserve in women with SCD. Although months of HU exposure was not associated with low AMH, HU exposure does not account for adherence, which is a major limitation in most sickle cell studies. MCV which increases with consistent HU use and is a biological proxy measure of the last 3-months of HU adherence, was associated with low AMH. Ovarian reserve was not a planned endpoint in the MSH. A prospective study of ovarian reserve in women with SCD is needed to understand how the physiology of SCD itself or exposure to HU may influence multiple fertility endpoints.
Chaturvedi:Shire/Takeda: Research Funding; Sanofi: Consultancy; Alexion: Consultancy. Lanzkron:PCORI: Research Funding; NIH: Research Funding; Pfizer: Research Funding; Global Blood Therapeutics: Research Funding; Ironwood: Research Funding; HRSA: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal