Abstract
Women with inherited bleeding disorders, including carriers of hemophilia A and B, or with von Willebrand disease, have an increased risk of bleeding during pregnancy and delivery. The unborn child may also be affected by the bleeding disorder for which specific measures have to be considered. This requires a multidisciplinary approach, with a team that includes a hematologist, a pediatric hematologist, a clinical geneticist, an obstetrician-perinatologist, and an anesthesiologist. An optimal approach includes prepregnancy genetic counseling, prenatal diagnostic procedures, and a treatment plan for delivery for both the mother and child. Recent retrospective studies show that even if strict guidelines are followed, these women are still at risk of postpartum bleeding. This occurs even if coagulation factor levels are normalized, either due to the pregnancy-induced rise of factor levels or by infusion of coagulation factor concentrates at the time of delivery. In this article, we describe our current diagnostic and clinical management of pregnancy and delivery in women with inherited bleeding disorders. We also briefly discuss possible interventions to improve the outcome of current strategies by increasing target factor levels during and after delivery.
Introduction
Carriers of hemophilia A (HA) or hemophilia B (HB) and women suffering from von Willebrand disease (VWD) have an increased risk for bleeding during pregnancy and delivery. Management of these women concerns not only managing the bleeding tendency of the mother, but also that of the child with a potential bleeding disorder. Hemophilia is an X-linked inherited bleeding disorder. Women are carriers and may have reduced factor levels. Carriers of hemophilia can be classified as obligatory carriers who certainly carry the affected X-chromosome, and possible carriers with a chance of having the affected X-chromosome. Moreover, new mutations occur quite frequently, and 30% to 50% of newborns with hemophilia are de novo cases.1,2 VWD is a more heterogeneous bleeding disorder, mainly autosomal-dominant inherited. Various types and subtypes are known, each with different inheritance, severity, and management.3
Hemostatic changes in healthy women during pregnancy and delivery
During pregnancy, the hemostatic balance is changing toward a procoagulant state in order to be prepared for blood loss during delivery and the postpartum period.4-8 This procoagulant state is caused by a physiological increase of many coagulation factors, including factor VIII (FVIII) and von Willebrand factor (VWF) with a peak shortly before giving birth.7 The procoagulant state is also characterized by a decrease of anticoagulant proteins and reduced fibrinolysis.5,7 Twelve weeks postpartum, these changes have returned to normal. The physiological increase in FVIII, VWF, and, to a lesser extent, FIX during pregnancy are relevant for the management of pregnant carriers of hemophilia and women with VWD.
Hemostasis in healthy newborns
Several studies have evaluated the postnatal development of the hemostatic system.7,9-11 At birth, the vitamin K–dependent coagulation factors and contact factors are ∼50% of normal adult values.11,12 However, VWF and FVIII are comparable to adult levels in the full-term neonate, and levels may be even higher shortly after birth.7,11 The low levels of procoagulant factors are counterbalanced by physiologically low anticoagulant proteins.10,13 As a result, thrombin generation is normal in healthy newborns.14,15
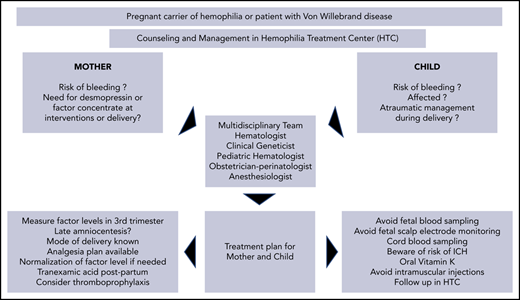
Pregnancy in women with bleeding disorders
In women with bleeding disorders, physiological procoagulant changes in hemostasis also occur. However, these are often insufficient to prevent bleeding. Therefore, women with a bleeding disorder should be counseled before pregnancy and followed during pregnancy; a treatment plan for delivery should be made. Because this requires expertise, they should be referred to specialized hospitals with a hemophilia treatment center. A multidisciplinary team including a hematologist, a pediatric hematologist, an obstetrician-perinatologist, a clinical geneticist, and an anesthesiologist with expertise in bleeding disorders should make a management plan for care during pregnancy and delivery for the mother and neonate. This treatment plan should be available for all involved professionals and should be shared with the woman from 34 weeks of gestation.
Pregnancy in hemophilia carriers
Case history
A 32-year-old nulliparous woman was referred to our clinic at 16 weeks of gestation. Her history revealed 2 surgeries without excessive bleeding. She was a carrier of HA because her father had severe HA. Her FVIII procoagulant activity (FVIII:C) was 35 IU/dL. Mutation analysis of the FVIII gene (F8)of her father revealed an inversion intron 22. Options for prenatal testing were discussed with the parents. She was referred to the obstetrician and at 20 weeks of gestation an ultrasound showed a male fetus. At 33 weeks, amniocentesis was performed (her FVIII:C was 105 IU/dL at 32 weeks) and revealed that the fetus had HA. A delivery plan was discussed in our multidisciplinary meeting. After an unassisted spontaneous vaginal delivery at 39 weeks, an otherwise healthy male neonate was born. Total blood loss during delivery was 300 mL. The next day, mother and son were discharged.
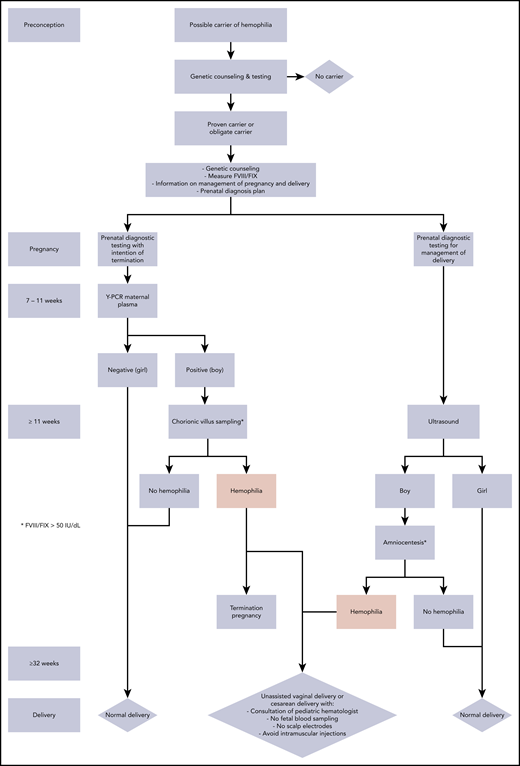
Ideally, all (potential) carriers undergo genetic testing to confirm the diagnosis of hemophilia and to establish the causative mutation. In addition, FVIII or FIX levels should be determined before pregnancy. Carriers should receive preconception counseling about the genetic transmission and the various methods to determine the sex of the fetus and in case of a male fetus, whether he is affected with hemophilia. With this information, the couple can reflect on the available reproductive options for prenatal diagnosis and the planning and management of pregnancy and delivery. Psychological support should be offered to parents of children born with bleeding disorders along with a consultation with a pediatric hematologist about the implications of taking care of a boy with hemophilia.
If, after preconception counseling, a couple decides they want to avoid the risk of having an affected child, we inform them about the possibilities of preimplantation genetic screening or antenatal genetic screening by chorionic villus sampling (weeks 10-14 of gestation) or amniocentesis (from week 15 of gestation) followed by (early) termination of pregnancy in case of an affected male fetus.16-18 The latter is only possible if the causative mutation is known and if the national laws governing such procedures make this possible.
If prenatal diagnosis is not performed, fetal sex determination is done by assessing Y-chromosome fetal DNA in maternal plasma (from 7-9 weeks of gestation) or by ultrasound (reliably possible from week 16 of gestation). A female fetus has a 50% chance of being a carrier. Because most female carrier newborns will have normal or only mild reduced FVIII/FIX levels and severe reduced factor levels are very rare, delivery of a (possible) carrier of hemophilia does not carry a risk of neonatal bleeding.17,18 A male fetus has a 50% chance of being affected with hemophilia. When the causative mutation is known, it is possible to determine antenatally whether the boy is affected or not by analyzing fetal DNA obtained by chorionic villus sampling or amniocentesis. The procedure-related risk of miscarriage is low to negligible.19 Besides, amniocentesis can be postponed until the third trimester because the result is only relevant for delivery. This so-called late amniocentesis can be performed with almost no complications.
The optimal mode of delivery for a hemophilia carrier expecting a (possibly) affected male neonate is often debated.20-22 The most feared complication is intracranial hemorrhage (ICH). In healthy children, the risk during vaginal, instrumental, or cesarean delivery is <0.2%, whereas studies in hemophilia-affected children reported incidence rates of 0.8% to 2.3%.23-25 A recent large study in hemophilia carriers showed a similar risk of ICH after planned vaginal deliveries (2.4%), which included instrumental vaginal deliveries, and cesarean deliveries (1.7%), including elective or planned and emergency procedures.26 Instrumental vaginal delivery, however, increased the risk of ICH almost sevenold. Another study in hemophilia carriers showed a 10-fold increased risk of ICH during instrumental vs spontaneous vaginal delivery.27 The UK guideline advises that the possibility of an elective cesarean delivery be discussed with carriers expecting a (potentially) (moderate) severe hemophilia male neonate.28 The US guideline recommends cesarean delivery for a (potentially) affected boy.29 It is important to note that cesarean delivery during labor does not eliminate the risk of ICH and may increase the risk of maternal bleeding, as well as the number of days in hospital and prolonged need for hemostatic treatment of the mother.30 Both delivery options should be considered and discussed by the obstetrician and the women during pregnancy.28
In The Netherlands, where the possibility of performing an emergency cesarean delivery within 15 to 30 minutes exists, these women are advised to deliver vaginally, but if the second stage of labor is prolonged or fetal distress is suspected, an emergency cesarean section will be performed.
What is our approach in a hemophilia carrier before and during pregnancy?
Ideally, the carrier is counseled before pregnancy, the causative mutation is determined, and FVIII/FIX levels are measured. We counsel the couple about all possible options as shown in Figure 1. During pregnancy, we assess the sex of the fetus by ultrasound. If the carrier is pregnant with a female fetus, no restrictions during delivery are advised, and the girl is seen within 1 year after birth (or earlier in case of intervention) by our pediatric hematologist. If the carrier is pregnant with a boy with (possible) hemophilia, the obstetrician discusses the pros and cons of the different modes of delivery and the anesthesiologist discusses the options for analgesia. Instrumental vaginal deliveries should be avoided as much as possible, but if unavoidable, forceps delivery is preferred over ventouse delivery.17 As mentioned earlier, we recommend an unassisted vaginal delivery with an early recourse to an emergency cesarean delivery if the second stage of labor is prolonged or there is suspected fetal distress.17,18 The use of potentially harmful invasive techniques, like fetal scalp electrodes or fetal blood sampling, is avoided, as well as intramuscular injections in the neonate after birth: this is so-called atraumatic management (Figure 1).
Algorithm for management of (possible) carriers of HA or HB. The approach to prenatal diagnostic testing is shown (left) when the intention is to terminate pregnancy in cases of (severe) hemophilia or (right) if diagnostic testing is performed with the intention of establishing the management of delivery.
Algorithm for management of (possible) carriers of HA or HB. The approach to prenatal diagnostic testing is shown (left) when the intention is to terminate pregnancy in cases of (severe) hemophilia or (right) if diagnostic testing is performed with the intention of establishing the management of delivery.
Managing the delivery in carriers of hemophilia
In hemophilia carriers, the median FVIII/FIX levels are 55 to 68 IU/dL, but these may range from <10 IU/dL to >100 IU/dL.31-33 If FVIII/FIX levels are below the hemostatic level (40-50 IU/dL), then the carrier needs hemostatic support during prenatal genetic diagnostic tests and delivery to reduce the risk of bleeding.34 As discussed earlier, FVIII levels increase during pregnancy twofold to threefold, whereas FIX levels increase only slightly.7,8,35,36 Carriers of hemophilia are at an increased risk for postpartum hemorrhage (PPH), not only those with low levels, but also those with normal FVIII/FIX levels.37,38 Retrospective studies reported PPH (>500 mL) in 19% to 48% of deliveries.35,36,39,40 For comparison, the incidence of PPH in low-risk nulliparous women in the Dutch general population is 19%, and of severe PPH (>1000 mL) 4.5%.41,42 In many guidelines on hemophilia carriers, factor levels in the third trimester ≥50 IU/dL are considered sufficient for delivery; below 50 IU/dL, administration of factor concentrates is warranted during delivery.17,18,28,29 As an alternative to FVIII concentrate, desmopressin (DDAVP) can be administered in carriers of HA. Desmopressin can be safely administered in the first and second trimesters of pregnancy, however, its safety has not been demonstrated at the time of delivery.43,44 If desmopressin is used, it should be administered after clamping the umbilical cord because of the possibility of hypotension in the mother, which may harm the child.45,46 Desmopressin has also been reported to cause neonatal hyponatremia,47 and can cause fluid retention, especially when oxytocin is also administered. Therefore, desmopressin should be used with caution, fluid should be restricted (if possible <1500 mL) for the first 24 hours in the postpartum period, and electrolytes and urine output must be monitored.28,29,45
What is our approach in a hemophilia carrier during delivery?
Based on the observed high prevalence of PPH, the Dutch guideline was recently updated with the aim of lowering the risk of bleeding by targeting higher factor levels at delivery.36,40 Therefore, the cutoff value of FVIII or FIX, measured in the third trimester for treatment with factor concentrates, was increased from 50 IU/dL to 80 IU/dL. In addition, the targeted peak level at delivery was increased from 100 to 150 IU/dL. After initial treatment, trough levels are kept >50 IU/dL for 3 days (vaginal delivery) and for 5 days (cesarean delivery). In addition, after delivery, we give 1 g of oral tranexamic acid 3 to 4 times daily for 7 days. Because our guideline differs from other international guidelines, outcome data will be prospectively collected and evaluated (Prides study; NCT NL6770 NTR6947).
Pregnancy in women with VWD
Case history
A 27-year old primiparous woman with VWD was referred to our department at 12 weeks of gestation. In her obstetric history, she had 2 miscarriages and 1 spontaneous vaginal delivery. Her first delivery was complicated by a PPH of 1000 mL despite infusion of FVIII/VWF concentrate before delivery (no data available on postinfusion factor levels). She had VWD type 2M (FVIII:C, 74 IU/dL; VWF antigen activity [VWF:Ag], 59 IU/dL; VWF mutant glycoprotein Ib–binding activity [VWF:GPIbM], 16 IU/dL; VWF collagen-binding activity, 62 IU/dL; normal multimer pattern). Mutation analysis revealed a heterozygous mutation in the VWF gene in exon 28: c.3877T>C p.Phe1293Leu. Factor levels were measured at 24 weeks of gestation and revealed increased FVIII:C (151 IU/dL) and VWF:Ag (117 IU/dL) levels, but a persistent low VWF:GPIbM of 11 IU/dL. At 33 weeks, amniocentesis was performed after administration of VWF/FVIII concentrate. Mutation analysis revealed that the fetus was not affected with VWD. Because of persistent low VWF:GPIbM in the third trimester, she received 40 IU/kg VWF ristocetin cofactor activity (VWF:RCo) FVIII/VWF concentrate before delivery (peak level VWF:GPIbM, 1.08 IU/dL). Because of a prolonged second stage of labor, a ventouse delivery was performed. A second-degree perineal laceration occurred and blood loss was 800 mL. FVIII/VWF concentrate was continued twice daily 20 IU/kg VWF:RCo for 3 days. One gram of oral tranexamic acid was prescribed 4 times daily for 7 days. She was discharged after 3 days and developed no secondary PPH.
As illustrated herein, women with VWD carry an increased risk of bleeding during pregnancy and especially during delivery.48 Our patient had experienced 2 bleeding episodes peripartum, both occurring despite infusion of VWF/FVIII concentrate. She also experienced 2 miscarriages. The precise risk of miscarriage in VWD is thus far unclear, but there are indications that the risk is not increased.48-50 In a cohort of 423 Dutch women with VWD, the mean number of children was 1.9, which is comparable to the general population (1.8).51 Similar numbers were reported for women with low VWF.52 It should be noted, however, that the number of live births is not predictive of the number of pregnancies and risk of miscarriages; as such, these data should be interpreted with caution.
There are important differences between the management of carriers of hemophilia and patients with VWD. VWD is a more heterogeneous bleeding disorder, with various types and subtypes, with different bleeding risks and also different management strategies. In addition, VWD is autosomal inherited, mainly dominant, which indicates that girls are equally as affected by VWD as boys. Given its complexity and the risk of bleeding in mother and child, monitoring and care of pregnant women with VWD should only be performed in hospitals with a hemophilia treatment center.
Prenatal genetic testing in VWD
In patients with VWD, genetic testing is not routinely performed because it is elaborate given the size of the gene and has, besides pregnancy, limited clinical implications. In patients with type 1 VWD, mutations may be distributed over the entire VWF gene. A mutation is found in over 90% in type 1 VWD patients with VWF levels <15 IU/dL, but is found in only 40% in patients with low VWF (defined as VWF 30-50 IU/dL).53,54 Therefore, genetic testing is frequently not informative in women with mild VWD type 1. In patients with type 3 or type 2 VWD, genetic testing may be considered and is more frequently performed today. In type 2 VWD, a mutation is found in over 90% of patients and is located in certain exons that are linked to the subtype of VWD.53
What is our approach in women with VWD before and during pregnancy?
Given the risk of 50% of having a child with VWD, women suffering from severe VWD should be counseled about not only having a child with VWD, but also the implications for pregnancy and mode of delivery. Genetic counseling is especially advised for parents who already have a child with type 3 VWD.55 By genetic testing of both parents, the causative mutations can be determined and, if early termination of pregnancy is considered, an affected child can be identified by chorionic villus sampling. In phenotypically milder types of VWD, termination of pregnancy is rarely considered. In patients in whom the causative mutation in VWF is known, we discuss the possibility of performing amniocentesis at 30 to 32 weeks of pregnancy to diagnose or rule out VWD in the fetus in order to make a treatment plan for delivery. Before performing late amniocentesis, the current levels of VWF and FVIII of the patient should be known. If these levels are <50 IU/dL, treatment is given with FVIII/VWF concentrate or desmopressin.
Managing delivery in women with VWD
In patients with low VWF or type 1 VWD, VWF and FVIII levels increase during pregnancy, especially in the third trimester.54,56 At the time of delivery, these levels can be 2 to 3 times higher compared with baseline levels. However, some women, even with mild-type 1 VWD, do not show this increase. In type 2 VWD patients, VWF:Ag and FVIII levels also increase during pregnancy, but functional VWF (VWF:RCo and/or VWF:GPIbM) remains low.57 Levels of VWF and FVIII in VWD type 3 remain low throughout pregnancy and the women should therefore always be treated with factor concentrate at delivery.58 Because of the unpredictable increase of levels during pregnancy, it is necessary to measure VWF:Ag, VWF:RCo (or VWF:GPIbM), and FVIII between 30 and 34 weeks of pregnancy. To prevent bleeding during delivery and postpartum, current guidelines for women with VWD state that if the functional levels of VWF and FVIII (VWF:RCo or FVIII:C) are <50 IU/dL during the third trimester, then desmopressin or IV VWF/FVIII concentrate should be administered during vaginal and caesarean delivery.57,59 Desmopressin can only be administered in women with a previously demonstrated good response to FVIII and VWF and should be used with caution as was discussed in “Managing the delivery in carriers of hemophilia.”
What is our approach for delivery in VWD?
In women with type 1 or 2 VWD who do not respond to desmopressin and in type 3 VWD patients, we administer FVIII/VWF concentrate before delivery. Only a minority of VWD patients in our center require treatment with factor concentrates at delivery and they are treated according to the current guidelines.36 Prolonged factor infusion for several days is administered to avoid long-term postpartum bleeding. We usually administer 40 to 60 VWF:RCo IU/kg as close to the delivery as possible, continued twice daily at 20 to 30 IU/kg for 3 to 5 days after vaginal delivery, and monitor levels of functional activity (VWF:RCo or VWF:GPIbM) and FVIII:C once daily. After cesarean delivery, we administer FVIII/VWF concentrate for at least 5 days
In recent years, many reported studies challenge the current guidelines on VWD management during delivery. Several studies showed that in women with type 1 VWD, PPH still occurs frequently despite the increase and normalization of endogenous VWF and FVIII.60 Several other groups have also reported high rates of PPH despite the use of concentrate to normalize FVIII and VWF levels.36,61,62 In these latter studies, VWD women who were administered predelivery FVIII/VWF factor concentrates, based on low levels of VWF/FVIII in the third trimester, had more blood loss compared with women without VWD or untreated type 1 VWD women. In a recent Dutch study, PPH was reported in more than 50% of VWD patients with VWF levels <50 IU/dL in the third trimester, despite treatment with VWF concentrate aiming at levels >100 IU/dL at delivery.36 These findings suggest that higher FVIII and VWF levels are needed to prevent bleeding in VWD women.60
In The Netherlands, we therefore recently changed our guideline: we now advise treating VWD women at delivery with desmopressin or factor concentrate if VWF activity (VWF:RCo) levels are <80 IU/dL in the third trimester and increasing the target peak level of VWF activity to at least 150 IU/dL. This management will be evaluated prospectively in the same study in hemophilia carriers (Prides study). Similar treatment strategies are now being investigated by others, also aiming for higher, more physiological levels at delivery by infusion of an increased VWF dose (VIP study; NCT 04146376).63,64
A specific group of women with VWD who deserve more attention are those with type 2B. Type 2B is characterized by low functional VWF levels, loss of high-molecular-weight multimers and thrombocytopenia, caused by specific gain-of-function mutations in the A1 domain of VWF. During pregnancy, severe thrombocytopenia may occur. Therefore, platelet counts should be assessed regularly during the third trimester, if there are bleeding symptoms, and at delivery. In addition to administration of VWF/FVIII concentrates at delivery, platelet transfusion is also recommended if platelet counts are <50 × 109/L.65,66
Care for the neonate with VWD
During delivery, bleeding complications may not only occur in the woman with VWD, but also in the affected child. In low VWF and mild type 1 VWD, this bleeding risk is negligible because VWF and FVIII levels are increased at birth, as has been demonstrated in healthy newborns.10,67 If it is known by prenatal diagnosis that the unborn child has type 2 or 3 VWD, we advise the earlier described atraumatic management. Several guidelines also recommend that an instrumental delivery not be performed because of the risk of bleeding in the affected neonate.57,68 A similar approach is advised for potentially affected children if prenatal diagnostics were not performed or were inconclusive. Recent studies have shown that neonates with severe VWD are at risk of bleeding. Although ICH is a very rare complication in patients with VWD,69 cephalohematoma was reported in 4 of 100 VWD children in a Canadian study and 11 of 113 children in the WiN study.70,71 This may also have important implications in men with severe VWD whose partner is pregnant. These children are also at risk of having VWD, and similar management during delivery should be advised. In women with type 3 VWD caused by double heterozygote mutation, an atraumatic delivery is not necessary because the heterozygous children have no severe bleeding phenotype. This may depend, however, on the underlying VWF mutations.55,72
Additional management issues in women with bleeding disorders
Locoregional anesthesia should be administered with caution. There are only a few reports on the use of neuraxial anesthesia in hemophilia or VWD patients with and without treatment with factor concentrates and the occurrence of spinal hematomas. It is generally accepted that FVIII/FIX or VWF levels in the normal range (>50 IU/dL) are sufficient to normalize the risk of a spinal or epidural hematoma to the risk in the general population (1 in 168 000 in obstetric patients after epidural anesthesia).73 We generally perform epidural anesthesia in hemophilia carriers and women with low VWF or type 1 VWD who have levels of FVIII and VWF:RCo > 50 IU/dL in the third trimester without additional measures. We maintain FVIII/FIX and VWF levels >50 IU/dL for the duration of catheter placement and for at least 12 hours (mild hemophilia) to 24 hours (moderate or severe hemophilia) after catheter removal.17,28,74 However, in the recent UK guideline, neuraxial anesthesia is not recommended for use in women with type 2 or 3 VWD irrespective of whether VWF activity has been restored to apparently normal levels.59
In carriers of hemophilia or women with VWD undergoing cesarean delivery receiving FVIII (/VWF) concentrate or desmopressin, we consider thrombosis prophylaxis with low-molecular-weight heparin during hospital stay or longer if there is prolonged immobilization, following the Dutch guidelines (https://richtlijnendatabase.nl/richtlijn/antitrombotisch_beleid). Women with major risk factors resulting in a postpartum thrombosis risk of >3% are given low-molecular-weight heparin.75 Thromboprophylaxis is given because normalization of VWF and FVIII levels in the postpartum period by administration of factor concentrate may result in a similar risk of postpartum thrombosis as in other women postpartum.57 In addition, prolonged factor replacement in patients with VWD may lead to high FVIII levels, leading to an even higher risk of venous thrombosis.76 This is in line with current American College of Obstetricians and Gynecologists (ACOG) guidelines, which recommend careful consideration of the risk of thrombosis and bleeding.77
Tranexamic acid has been shown to decrease PPH in women without bleeding disorders.78,79 It also lowers the risk of PPH in women with bleeding disorders and does not increase the risk of thrombosis after vaginal or cesarean delivery.80-82 We prescribe tranexamic acid for at least 7 days postpartum for all women with bleeding disorders. After delivery, VWF and FVIII levels will gradually decrease to baseline levels within 3 weeks postpartum, and these women are prone to delayed bleeding in the puerperium.61,83 Tranexamic acid can be safely prescribed to breastfeeding women.80
Final remark
We are aware that our view is based on providing counseling and care in a well-functioning medical system, and that the diagnostic and treatment options mentioned in this article may not be available in all countries. However, in developing countries also, informing women with bleeding disorders about the risk of bleeding during childbirth and the risk of giving birth to a child with bleeding problems is of the utmost importance.
Authorship
Contribution: F.W.G.L., J.D., and M.J.H.A.K. wrote the paper.
Conflict-of-interest disclosure: F.W.G.L. received unrestricted research grants from CSL Behring, Shire/Takeda, Sobi, and uniQure; is a consultant for CSL Behring, Shire/Takeda, Biomarin, and uniQure, fees for which go to the university; is a member of the data safety monitoring board of a study sponsored by Roche; and received a travel fee from Sobi. M.J.H.A.K. received unrestricted research grants from Pfizer, Bayer, Daiichi Sankyo, Sobi, and Boehringer Ingelheim and a speaker’s fee from Bayer, fees for which go to the university. J.D. declares no competing financial interests.
Correspondence: Frank W. G. Leebeek, Department of Hematology, Erasmus MC, University Medical Center Rotterdam, Room Na822, Dr Molewaterplein 40, 3015 GD Rotterdam, The Netherlands; e-mail: f.leebeek@erasmusmc.nl.