Even in ugly diseases like mantle cell lymphoma (MCL), it is impossible to ignore the beauty of the logical order regulating biological processes: kinases are regulated by phosphorylation, protease activity by proteolytical cleavage, and so forth. In this issue of Blood, Pararajalingam et al identified perturbed RNA processing due to alternative splicing from somatic mutations in intronic regions of a gene that encodes for an RNA binding protein (HNRNPH1 [Heterogeneous Nuclear Ribonucleoprotein H1]) in MCL.1 This adds another candidate to the growing list of alterations that determine the heterogeneous biology, distinct clinical courses, and differences in treatment outcomes of patients with this disease.
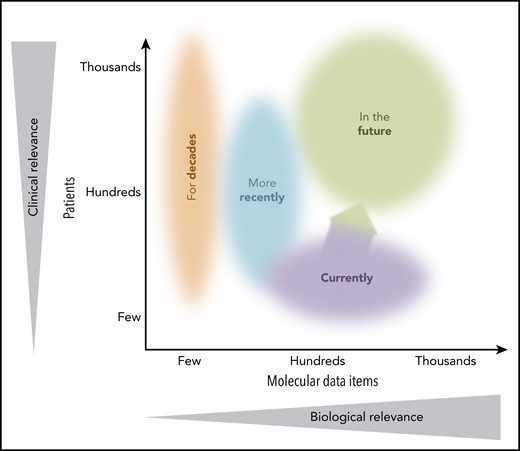
Schematic diagram of scope in translational research. Arrow illustrates that the study by Pararajalingam et al marks the beginning of comprehensive molecular profiling in clinically meaningful numbers of patients with MCL.
Schematic diagram of scope in translational research. Arrow illustrates that the study by Pararajalingam et al marks the beginning of comprehensive molecular profiling in clinically meaningful numbers of patients with MCL.
MCL comprises <10% of all mature B-cell non-Hodgkin lymphomas, but poses substantial diagnostic and clinical challenges. Hematopathologists distinguish classical MCL from several less common variants by morphology, immune phenotype, and immunohistochemistry. Hematologists use the clinical presentation to distinguish nodal MCL from rare nonnodal/leukemic variants. Most, but not all, MCL carry the hallmark translocation t(11;14)(q13;q32), which places the protooncogene CCND1 (which encodes for cyclin D1) under the control of the immunoglobulin heavy chain enhancer. The landscape of recurrent genetic, genomic, and epigenomic alterations is highly complex,2-4 providing the ultimate evidence of the biological heterogeneity of this disease.
Determining the relevant complement of molecular alterations that drive the individual phenotype of MCL (and other cancers) is a clinical priority. The benefits of defining these molecular alterations include improved diagnostic precision and prognostication, optimized patient stratification, informed treatment decisions, as well as identification and targeting of novel therapeutic vulnerabilities.
In translational research, size matters. Conceptually, the more cases analyzed, the higher the clinical relevance. The more comprehensive the molecular profiles, the higher the biological relevance (see figure).
Decades of research have established a handful of distinct prognostic biomarkers with robust clinical relevance by examining large cohorts of patients. Examples include high proliferation rate by Ki67 labeling indexing5 or gene expression profiling,6 high TP53 protein expression,7 as well as TP53 mutations and deletions.8,9 More recent efforts include analysis of hundreds of cases by more focused DNA sequencing,10 or dozens of cases by more comprehensive molecular profiling.2-4
The study by Pararajalingam et al complements these prior studies by analyzing a total of 272 primary MCL tumors using whole-genome sequencing, whole-exome sequencing, or targeted DNA sequencing, along with RNA sequencing in a subset of samples (n = 103). This study marks the beginning of comprehensive molecular profiling in clinically significant numbers of patients (see figure). As such, this study constitutes a highly valuable resource for future research. Among other findings, this study confirmed that some gene mutations (eg, TP53 and NOTCH1)3,9 were associated with shorter overall survival in a subset of patients who received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone; n = 133), while other gene mutations that have previously been reported to have prognostic value (eg, KMT2D, NOTCH2)3,10 were not. This illustrates that despite the impressive size of this study, further studies in homogeneously treated cohorts are needed to validate and expand on these findings and to address factors like patient selection and treatment context, especially since R-CHOP is no longer considered standard of care for most patients with MCL.
The most remarkable finding of the current study, however, is the identification of recurrent and significant mutations in genes that encode for regulatory RNA-binding proteins. This includes HNRNPH1, which was mutated in 10% of cases when both coding and noncoding mutations were considered. HNRNPH1 is involved in regulation of alternative pre-mRNA splicing. HNRNPH1 itself can be alternatively spliced, and exclusion of its exon 4 is associated with nonsense-mediated decay and lower HNRNPH1 protein levels. Pararajalingam et al noted that the somatic mutations in HNRNPH1 were actually mostly intronic, peculiarly clustered in regions flanking exon 4. RNA sequencing showed no differences in HNRNPH1 mRNA levels, but skewing of transcripts toward inclusion of exon 4 in the presence of these intronic mutations was found. Although the precise molecular mechanism still needs to be worked out, the authors showed that these intronic mutations favor inclusion of exon 4, leading to increased levels of HNRNPH1 protein levels. Interestingly, the authors showed that a higher ratio of unspliced-to-spliced exon 4 HNRNPH1 transcripts (“splicing ratio”) significantly correlated with shorter overall survival in patients receiving R-CHOP, while HNRNPH1 mutation status alone did not.
Trivial but true, good research raises new questions: If HNRNPH1 splicing ratio correlates with treatment outcome, yet HNRNPH1 mutations do not, what other alterations, other genes, or other mechanisms do contribute to inclusion of exon 4? Furthermore, what are the downstream effects of this skewed HNRNPH1 splicing ratio and increased HNRNPH1 protein levels (i) on other splicing events and the overall transcriptional landscape, and (ii) on a functional level? Last but not least, what is the prognostic or predictive impact of these alterations with other treatment regimens and in other lymphomas, and can this be exploited therapeutically?
In summary, Pararajalingam et al tackle the next level of translational research in MCL, including the assessment and functional characterization of the noncoding genome. This is the way to go, and there is more to come.
Conflict-of-interest disclosure: O.W. declares no competing financial interests.