BACKGROUND
Autologous Hematopoietic Stem Cell Transplant (AHSCT) remains an important treatment for multiple myeloma (MM) despite the continuous addition of novel agents into the therapeutic armamentarium. Since MM is predominantly a disease of the elderly, a significant proportion of patients do not undergo AHSCT due to 'a perceived lack of fitness'. This retrospective study evaluates the patterns of AHSCT in MM patients with regards to age and objective fitness assessment as per standardized indices.
METHODS:
Records of all MM patients treated at our institute from January 2017 till December 2019 were utilized to collect data regarding age, survival duration, risk scores as per the Revised-Myeloma Comorbidity Index (R-MCI) and fitness scores as per the Hematopoietic Stem Cell Transplant-Comorbidity Index (HSCT-CI). Patients with low and intermediate R-MCI risk scores were regarded as 'fit for AHSCT'. Patients with HSCT-CI categorizations of 'fit' and 'intermediate fit' were regarded as 'fit for AHSCT'. Proportions were compared using the Fisher-Exact-Test with a significance cut-off of p<0.05. Survival data were compared with the Log-Rank test.
RESULTS:
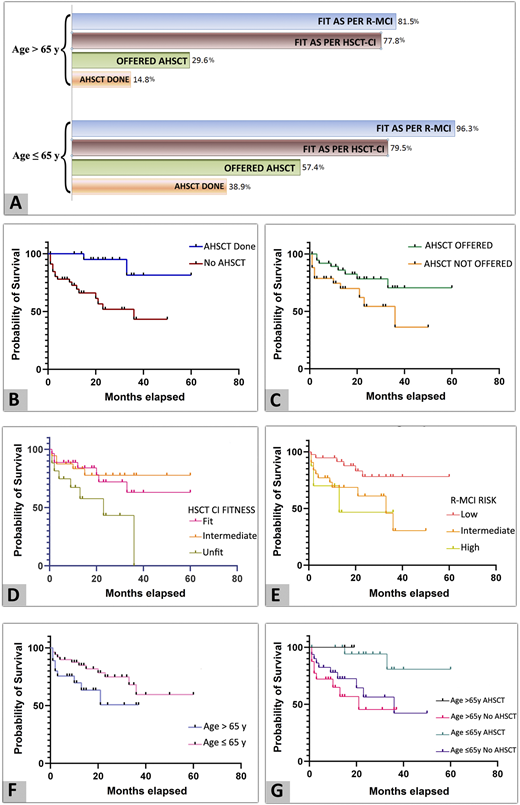
Out of the 81 patients, 54 (66.7%) were aged ≤65 years & 27 (33.3%) >65 years. The R-MCI classified 96.3% and 81.5% of patients aged ≤65 years and >65 years as AHSCT eligible, respectively (p 0.0381). The HSCT-CI classified a similar proportion of patients aged ≤65 years and >65 years as AHSCT eligible (79.6% vs. 77.8%, p 1). However, patients aged ≤65 years were offered AHSCT more frequently than those >65 years (57.4% vs. 29.6%, p 0.0207). Those aged ≤65 years underwent AHSCT more frequently than those >65 years (38.9% vs. 14.8%, p 0.0402). (Panel A, Figure-1).
Those who underwent AHSCT had greater median survival (MS) compared to those who did not undergo AHSCT (MS not reached vs. 36 months, p 0.0023) (Panel B, Figure 1). Those who were offered AHSCT had greater MS compared to those who were not offered AHSCT (MS not reached vs. 36 months, p 0.033) (Panel C, Figure 1). The MS of patients classified as fit and intermediate fit as per the HSCT CI was significantly better than that of those classified as 'unfit' (p 0.0362) (Panel D, Figure 1). The MS of patients classified by the R-MCI as low risk was significantly better than that of those classified as 'intermediate and high risk' (p 0.0253) (Panel E, Figure 1).
When the MS of overall patients aged ≤65 years was compared to that of those aged >65 years, there was no significant difference with the MS not reached in either group (p 0.0875) (Panel F, Figure 1).
When the survival curves of four groups (aged >65 years who underwent AHSCT, aged >65 years who did not undergo AHSCT, aged ≤65 years who underwent AHSCT, and those aged ≤65 years who did not undergo AHSCT) were compared, there was a statistically significant difference favouring those who underwent AHSCT irrespective of the age group (p 0.0167) (Panel G, Figure 1).
Conclusions:
Both the R-MCI and HSCT-CI revealed that approximately four out of five patients aged >65 years were AHSCT eligible. This analysis of the patterns of AHSCT for MM in our institution revealed a bias against those aged >65 years, with fewer patients of this age group being offered AHSCT. It would hence be prudent to perform objective fitness assessments using validated indices so as to ensure that every patient fit enough to benefit from an AHSCT receives the same irrespective of his/her age.
While it is well known that treatment availability and affordability are two major reasons for low rates of AHSCT in Low & Middle Income Countries (LMICs), it can be said from our data that physicians' bias against advanced age could be another factor. These results strongly suggest that use of AHSCT in fit elderly patients in LMICs may further improve outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal