Introduction:
Since its approval in 2014, ibrutinib has replaced chemotherapy to become a preferred therapy for CLL patients. Real-world studies of ibrutinib in CLL patients have shown higher rates of discontinuations due to adverse events (AEs; 14-23%) compared with data from the early clinical trials of ibrutinib (4-9%). Similarly, dose reduction rates due to AEs in the real-world studies were 22-28%, vs 9% in the ibrutinib package insert. These real-world studies have been mostly focused on the academic setting or based on registry data. This study was part of an initiative to collect chart-review data from an academic practice and broader community networks, using an identical protocol to describe ibrutinib dose reductions and discontinuations in CLL patients.
Methods:
This was a multicenter, retrospective, chart review study of CLL patients and treated with ibrutinib. De-identified data were pooled from 2 community networks and 1 academic practice. Each community network agreed to contribute 50 patients on ibrutinib to the pooled data. To minimize potential bias, the patients were randomly selected from all the ibrutinib-treated patients in each network. All patients meeting inclusion criteria from the academic site were included. Inclusion criteria were: confirmed diagnosis of CLL, initiation of ibrutinib between March 2014 and June 2019, and ≥18 years of age at the initiation of therapy. Patients were excluded if they were actively receiving therapy for other primary cancers or were enrolled in a clinical trial of ibrutinib during the study period. Index date was defined as the date of ibrutinib initiation, and patients were followed for a minimum of 6 months. Variables collected included: patient demographics, clinical and treatment characteristics, molecular profiles, and reasons for dose reduction and discontinuation. Descriptive statistics were used to summarize the results.
Results:
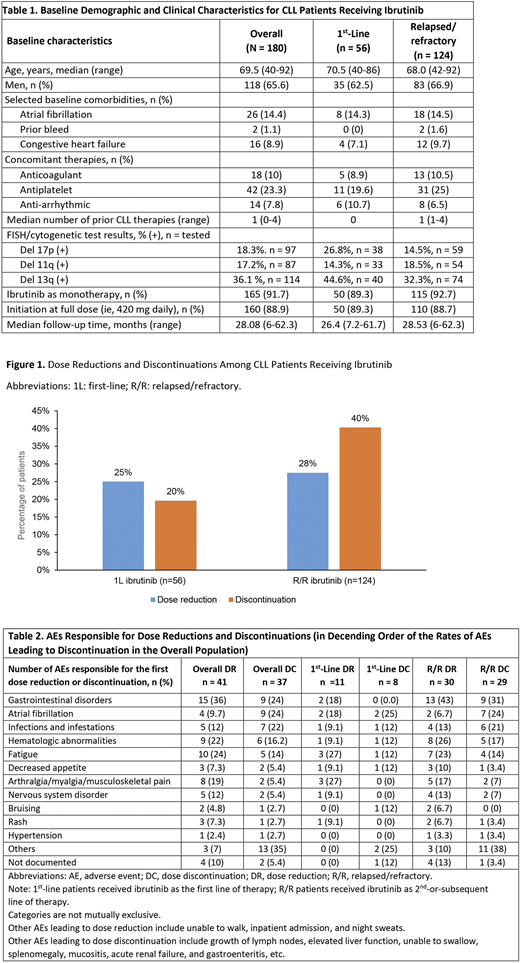
180 CLL Patients were included in this analysis. Of these, 56 (31%) patients received ibrutinib in the first line (1L) and 124 (69%) patients received ibrutinib in a relapsed/refractory (R/R) line. Over half (56%) of patients were treated in a community setting. Baseline demographic and clinical characteristics are shown in Table 1.
1L Ibrutinib patients had a median follow-up of 26 months. Twenty-five percent of patients (n=14) experienced at least one dose reduction, mainly due to AEs (n=11, 79%) (Figure 1). There was no single AE primarily responsible for dose reduction (Table 2). Treatment discontinuations were reported in 20% of patients, and they were more commonly due to AEs (73%) than disease progression (9%). Similarly, a variety of AEs led to discontinuations (Table 2). Median time to the first dose reduction for 1L patients was 9.9 months. Among patients who discontinued ibrutinib, median duration of treatment (DOT) was 15 months; with median DOT of 6 months for those who discontinued because of AEs and 28.9 months for those who discontinued because of progression.
R/R Ibrutinib patients had a median follow up of 28.5 months. About a quarter (27.5%, n=34) of patients experienced at least 1 dose reduction, mainly due to AEs (n=30 [88%]) (Figure 1). The most common AEs leading to the first dose reductions were gastrointestinal (GI) disorder (43%), fatigue (23%), , and arthralgia/myalgia/musculoskeletal pain (17%) (Table 2). Treatment discontinuation was reported in 40% of patients, with over half due to AEs (58%) rather than disease progression (18%). The most common AEs leading to discontinuation were GI disorders (31%), atrial fibrillation (24%), and infections (21%) (Table 2). Median time to the first dose reduction in R/R patients was 3.1 months. Among patients who discontinued ibrutinib, median DOT was 9 months; with median DOT of 6 months for those who discontinued because of AEs and 30.2 months for those who discontinued because of progression.
Conclusions:
Dose reductions and discontinuations were frequent in CLL patients receiving ibrutinib in routine clinical practice. Compared with ibrutinib clinical trial data at a similar follow-up time, AEs were the most common reasons leading to discontinuation of ibrutinib rather than disease progression. The rates of dose reduction and discontinuations due to AEs in our study were higher than in clinical trials and were consistent with other real-world studies, indicating similar patterns in both community and academic settings.
Hou:Verastem: Membership on an entity's Board of Directors or advisory committees; Genentech: Consultancy, Other: PI; AbbVie: Consultancy, Other: PI; AstraZeneca: Membership on an entity's Board of Directors or advisory committees, Research Funding. Ryan:AstraZeneca: Current Employment, Current equity holder in private company. Du:AstraZeneca: Other: Grant. Fang:AstraZeneca: Other: Grant. Marks:Sanofi: Research Funding. Page:AstraZeneca: Other: Grants. Peng:AstraZeneca: Other: Grant. Szymanski:AstraZeneca: Current Employment, Other: Stockholder. Le:AstraZeneca: Current Employment, Current equity holder in private company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal