Background
The Coronavirus disease-2019 (COVID-19) is a global pandemic caused by novel coronavirus SARS-CoV-2. Acute respiratory and renal failure as well as systemic coagulopathy are critical aspects of the morbidity and mortality in patients with COVID-19. Heparin Induced Thrombocytopenia (HIT) occurs when IgG antibodies form against platelet factor 4-Heparin complex, resulting in platelet activation and removal, leading to a prothrombotic state. HIT is suspected when there is a platelet count decrease of more than 50% after exposure to heparin, along with hypercoagulability. Clinical Scoring systems like 4T Score (Thrombocytopenia, Timing, Thrombosis, no other cause of Thrombocytopenia) have been developed to assess the pretest probability of HIT. The use of unfractionated heparin, post-orthopedic and post-cardiac surgery state, female gender, and old age are recognized as risk factors for HIT. There is a nine-fold increased risk of developing HIT in patients requiring hemodialysis. ICU patients and patients with VTE without thrombocytopenia are considered to have low pre-test probability for HIT. Studies have shown that only 6% who are investigated serologically for HIT actually have the diagnosis. We conducted this study to assess the incidence and risk factors for HIT in COVID-19 positive patients and its impact on mortality.
Methods
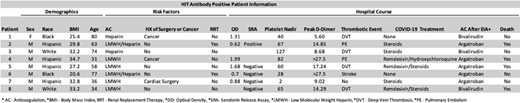
A retrospective analysis was performed on all patients who were COVID-19 positive and hospitalized between March 1, 2020 and June 26, 2020 at our institution. Patients with intermediate or high suspicion for HIT, based on 4T score of 4 or higher, underwent IgG-specific platelet factor 4(PF4)-dependent enzyme immune assay (EIA). Washed platelet assays such as serotonin release assay (SRA) and heparin-induced platelet aggregation (HIPA) were used as confirmatory tests in cases with intermediate or low optical density (OD) with EIA. The incidence of HIT, its impact on mortality, and positivity of IgG-specific PF4-EIA in COVID-19 patients were studied, and statistical analysis was done with X2 testing. Subgroup analysis was performed based on demographic factors and risk factors for HIT, including exposure to heparin or low molecular weight heparin (LMWH), history of or cancer, recent orthopedic or cardiac surgery, exposure to renal replacement therapy (RRT), and severity of disease (D-dimer >6 ULN, Acute Kidney Injury, ICU admission, and mechanical ventilation requirement). These factors were analyzed by Fisher's exact test to determine their impact on mortality. The hospital course for HIT antibody-positive patients was further analyzed to study the impact of COVID-19 related therapy, such as Remdesivir, Tocilizumab, Hydroxychloroquine, Steroids, and anticoagulation after diagnosis of HIT.
Results
WEight out of 1265 hospitalized COVID-19 positive patients tested positive for IgG-specific platelet factor 4(PF4)-dependent enzyme immune assay (EIA+). Incidence of EIA+ in COVID-19 patients was 0.6%, which is significantly higher than in the general population 0.2% (p<.0001, 95% CI 0.25-1.20%). The incidence of thromboembolic events in EIA+ patients was 87.5%, significantly higher than the rate of 10.90% in all COVID-19 patients (p<.0001, CI 41.96- 86.98%). The mortality rate in EIA+ patients was 50%, significantly greater than the mortality rate of 12% in all hospitalized COVID-19 patients (p=.0011, CI 9.46-66.53). Serological confirmation of HIT diagnosis was 37.5% (2 had OD>1, 1 was SRA positive) which is significantly higher than confirmation of HIT in nonCOVID-19 patients 6% (p<.0001, 95% CI 29.57-85.32%). All 3 confirmed HIT patients (100%) had severe disease (3/3 required ICU admission, 2/3 required mechanical ventilation, the one not requiring mechanical ventilation required RRT).
Conclusion
Our study indicates incidence of HIT is higher in the COVID-19 population. The incidence of positive EIA for patients with intermediate to high 4T scores is also higher in COVID-19 positive patients. This can be attributed to the cytokine storm and severe sepsis seen in critically ill COVID-19 patients. Our study also suggests that development of HIT can contribute to increased risk for thromboembolic events as well as mortality of COVID-19 patients, however, our study is limited due to small sample size. Therefore, prospective studies are needed to analyze the impact of HIT on morbidity, mortality and long-term outcomes in COVID-19 patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal