Introduction: Ph-negative myeloproliferative neoplasms (MPNs) are a group of clonal stem-cell disorders with an elevated risk for thrombosis. Leukocytosis is a well-known risk factor for thrombosis. Neutrophils from MPN patients display features of activation. On stimulation, neutrophils produce neutrophil extracellular traps (NETs), which have been implicated in the pathogenesis of thrombosis. Myeloperoxidase-conjugated DNA levels (a specific NET marker) have been found increased in plasma of thrombotic MPN patients (Guy, A, ISTH 2019 OC 77.3). Ex vivo, activated neutrophils from JAK2V617F patients are primed to form NETs, diminishing under ruxolitinib treatment. Mice with conditional knock-in of JAK2V617F have increased NETs formation and thrombotic events. Inhibition of JAK/STAT signaling by ruxolitinib abrogated NETs formation and reduced thrombosis in this murine model (Wolach, O,Sci. Transl. Med. 2018). Thus, a link between JAK2V617F expression, NETs formation and thrombosis has been suggested (Wolach, O, 2018). It remains unclear whether, in MPN patients, JAK/STAT independent pathways are implicated in the NETs formation. With this aim, we explored the effects of different cytoreductors in NETs formation.
Patients and Methods: In a multicentric study conducted at Hospital General Universitario Morales Meseguer (Murcia, Spain) and Hospital del Mar (Barcelona, Spain), EDTA plasma samples were collected from MPN patients (n=104). Patients include polycythemia vera (PV, n=35, all of them JAK2V617F), essential thrombocythemia [ET, n=47; 38 JAK2V617F, 4 CALRmut, 5 triple negative (TN)], myelofibrosis (MF, n=9; 4 JAK2V617F, 2 CALRmut, 3 TN), and unclassifiable MPN by WHO-2016 (MPN-u, n=13; 12 JAK2V617F, 1 CALRmut). Samples were collected at different time points following up the disease: at diagnosis or before any cytoreductive treatment, time 0, (n=100), less than 6 months of treatment (time 6; n=60), from 6 to 12 months of treatment (time 12; n=60), and from 12 to 24 months of treatment (time 24; n=49). Among the 104 patients, we had clinical information about treatment on 99 cases, included hydroxyurea (HU, n=69), ruxolitinib (n=15), IFN-α (n=2), and non-treated (n=13, all basal samples). We measured citH3-DNA complexes, as specific marker of NETs, by ELISA using rabbit anti-citH3 (Abcam) and peroxidase-conjugated anti-DNA antibody (Cell Death Detection ELISA). The absorbance at 405 nm (A405) was measured in a plate reader (Biotek®). Thus, we followed up the NETosis marker evolution with treatment over time. One-tailed and paired Wilcoxon test was applied and p<0.05 was taken as statistical significance.
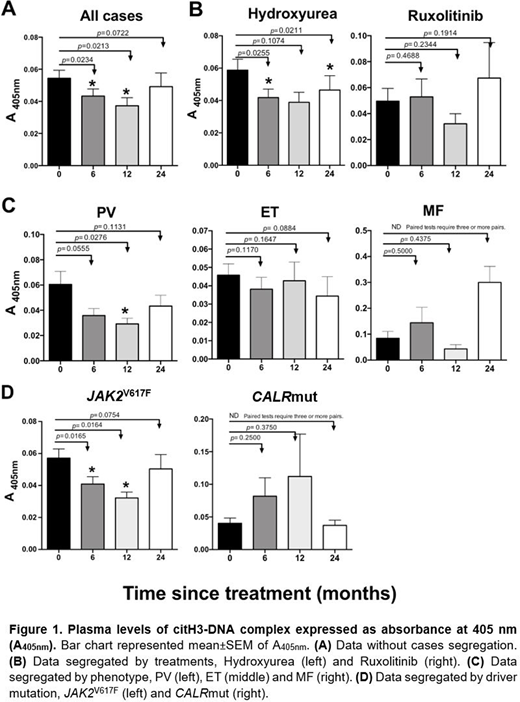
Results: Overall, regardless of the treatment, we observed a reduction of citH3-DNA levels over time (Fig. 1A), being these significant between time 0 and times 6 and 12 (p=0.02 for both time-points), Importantly, patients treated with HU showed a substantial reduction of NETs in all time-points (Fig. 1B, left), which was statistically significant between times 0 and 6 (p=0.03) and between times 0 and 24 (p=0.02). Although in patients treated with ruxolitinib, the citH3-DNA levels seem to be reduced at time 12, the difference was not significant (Fig. 1B, right), probably because of the small sample size. Regarding the MPN phenotype, decrease of citH3-DNA levels over time was only observed in PV patients (Fig. 1C, left), specially at time 12 (p=0.03). In contrast, under cytoreductive treatment, ET patients did not show significant differences in NETs levels over time (Fig. 1C, middle). In MF, there were not enough samples to obtain a clear conclusion (Fig. 1C, right). Regarding the driver gene mutations, we detected a significant decrease in the citH3-DNA levels in JAK2V617F patients (Fig. 1D, left), specifically between basal time and times 6 and 12 (p<0.02 for both time-points). Unfortunately, there are not enough samples to obtain a clear conclusion in CALRmut (Fig. 1D, right) and TN patients.
Conclusions: Our results showed that hydroxyurea reduces NETosis levels in plasma from MPN patients, suggesting that JAK-STAT independent pathways could be implicated in the NET formation. Hydroxyurea could decrease thrombosis in MPN patients, not just reducing the number of functionally abnormal cells in peripheral blood, but also by abrogating NET formation.
Acknowledgements: This study was supported in part by ISCIII (PI18/00316 & PI16/0153) & Fundación Séneca (20644/JLI/18).
Bellosillo:Qiagen: Consultancy, Speakers Bureau; Roche: Consultancy, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal