Introduction: Older adults with MM continue to remain under-represented in clinical trials, leading to paucity of information regarding the clinical characteristics and treatment outcomes, particularly among those 80y or older at the time of diagnosis. The International Myeloma Working Group (IMWG) classifies any patient >80y as frail, irrespective of their fitness status. The value of geriatric assessment and frailty evaluation in this subgroup remain unclear.
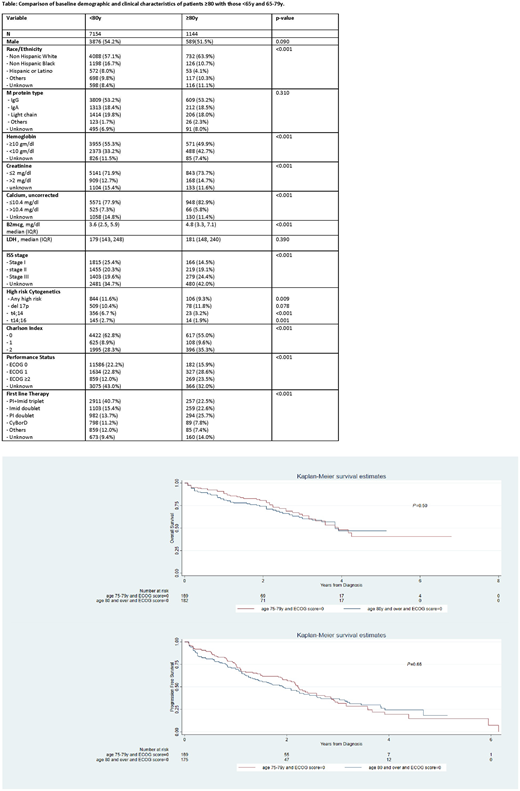
Methods: We used the Flatiron Health electronic record-derived de-identified database to source patients with incident MM diagnosed between January 1, 2011 and February 1, 2020. We compared clinical and demographic characteristics of patients ≥80y at the time of diagnosis with patients who were <80y of age. We abstracted baseline labs and cytogenetic data documented within 90 days from the start of first-line therapy. For those ≥80y, we captured the receipt of first line anti-myeloma therapy and examined early mortality (death within 6 months of diagnosis), derived progression-free survival (dPFS) and overall survival (OS) using Kaplan-Meier methods and Cox multivariate regression, with date of diagnosis as the index date. Finally, we compared dPFS and OS among potentially fit ≥80yo MM vs those between 75-79y, using ECOG performance status (PS) of zero as a surrogate marker of fitness status.
Results: Of 8298 MM patients in this cohort, 1144 (13.5%) patients were ≥80y at diagnosis (median 81y, range 80-85y). Compared with the younger cohort, those ≥80y were more likely to be white, and have anemia, renal insufficiency, higher β2-microglobulin and higher stage at diagnosis. However, there was a lower prevalence of documented high-risk cytogenetic abnormalities, particularly high risk translocations (t4;14 and t14;16) even after adjusting for race/ethnicity (Mantel Haenszel OR=0.67; p 0.001). Common first line therapies included proteasome inhibitor (PI) + Immunomodulatory agent (Imid) based triplet (23%), Imid doublet (21%) and PI doublet (27%) (Table). Patients ≥80y received a median of 1 (IQR 1-2) lines of therapy, as opposed to those <80 (median 2, IQR 1-3). Overall, the outcome was significantly inferior among the ≥80y patients be those <80y (median dPFS 16 vs. 39 months, p<0.01; median OS: 26 vs 37 months, p<0.01; and 6-month mortality rate: 20.1% vs 6.2%, p<0.01). However, patients ≥80y and ECOG PS of 0 had similar 3y-dPFS (36.8 vs 33.1%; p=0.66) and 3y-OS (61.8 vs 65.2%; p=0.50) when compared to those between 75-79y with similar PS (ECOG PS of 0) (Figure).
Conclusion: Patients 80y or above with newly diagnosed MM have distinct clinical and treatment characteristics as compared to their younger counterparts. Similar survival outcomes between older adults with good performance status vs their younger fit counterparts suggest the need for conducting a comprehensive frailty evaluation and individualized decision-making even in this cohort.
Giri:Carevive Systems: Honoraria; Pack Health: Research Funding; Carevive Systems: Research Funding. Costa:Celgene: Consultancy, Honoraria; BMS: Consultancy, Honoraria; Genentech: Consultancy; Janssen: Consultancy, Honoraria, Research Funding; Amgen: Consultancy, Honoraria, Research Funding; AbbVie: Consultancy; Sanofi: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal