Introduction
COVID-19 is an ongoing pandemic that has impacted millions of individuals throughout the world. The spectrum of clinical features of COVID-19 can vary from asymptomatic infection to severe multiorgan failure leading to death. There is no single biomarker available that can predict the trajectory of the infected patient. Few clinical reports suggest a correlation between the severity of COVID-19 and elevation of certain hematological and inflammatory markers. We used a novel COVID-19 Prognostic Score (CPS) which included lymphocyte count, elevated lactate dehydrogenase (LDH), C-reactive protein (CRP) and ferritin levels to predict the outcomes of COVID-19 patients.
Methods
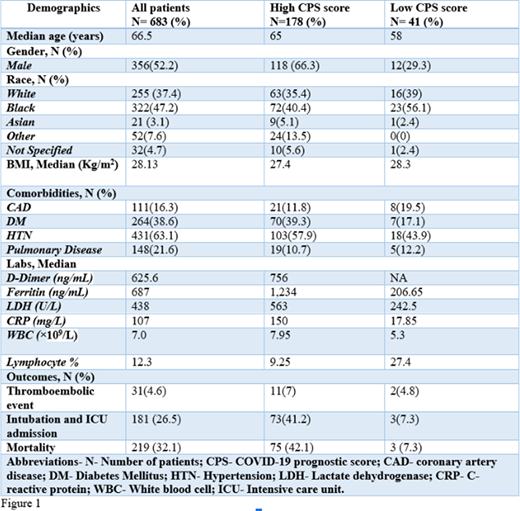
We performed a retrospective chart review of COVID-19 patients admitted to New York Presbyterian Brooklyn Methodist Hospital between March and April of 2020. Clinical data was extracted manually from electronic medical records. Patients were divided into 2 cohorts. The first cohort included a combination of low lymphocyte count, elevated LDH, CRP and ferritin. The second cohort included normal lymphocyte count, low LDH, CRP and ferritin. Low lymphocyte count was defined as < 20% of white blood cell count (WBC), high LDH as ≥ 300 U/L, high CRP as ≥50mg/L and high ferritin as ≥600 ng/mL. Statistical analysis was performed by computing odds ratio using a p-value of < 0.05 as statistically significant.
Results
We analyzed 683 hospitalized patients who were diagnosed with COVID-19 confirmed via viral PCR resting. The median age was 66.5 years, males were 52.2% and blacks were 47.2%. 16.3% had coronary artery disease (CAD), 38.6% had Diabetes Mellitus (DM), 63.1% had hypertension and 21.6% had pulmonary disease. 181 patients (26.5%) were intubated and transferred to ICU. The median LDH was 438 U/L, the median CRP was 107 mg/L and the median ferritin was 687 ng/mL. 4.6% of patients developed a thromboembolic event. The overall inpatient mortality rate was 32.1%. There were 178 patients in the CPS-High cohort while there were 41 patients who qualified for the CPS-Low cohort. The median age of CPS-High was 65 years and the median age of CPS-Low was 58 years. The percentage of CAD, DM, hypertension, pulmonary disease in CPS-High and CPS-Low were 11.8%, 39.3%, 57.9%, 10.7% and 19.5%, 17.1%, 43.9%, 12.2% respectively. In the CPS-High cohort the overall inpatient mortality was 42% while the inpatient mortality rate for CPS-Low was 7.3%. In univariate analysis, patients who had CPS low had significantly reduced inpatient mortality (Odds ratio 0.108, 95% CI 0.03-0.36, p-value = 0.0003).
Discussion
Our study suggests that a combination of hematological characteristics and inflammatory markers can be used to assess the severity of illness with COVID-19. This study shows that there is a likelihood of 6-times higher mortality with COVID-19 if all the clinical characteristics are abnormal including lymphocyte count, LDH, CRP, and ferritin. This simple clinical prognostic score can be used at the time of hospital admission to efficiently triage patients, which may likely improve the outcomes of these patients. This prognostic tool needs to be validated in a larger dataset or prospective clinical study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal