Background: Acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) are hematologic malignancies characterized by clonal myeloid expansion in the peripheral blood, bone marrow, and/or other tissues. During the past several years, the number of available FDA approved therapies for AML has dramatically increased, and multiple novel therapies for AML and MDS are in the pipeline. Not all patients will respond to these therapies, and early molecular markers of sensitivity vs resistance could facilitate selection of initial therapies or enable therapeutic pivots and personalization of treatment. Therefore, a sensitive method is required that will enable rapid identification of patients who are likely to benefit (or not benefit) from a therapy. In this study, we explore the feasibility of ex vivo drug screening to predict sensitivity and resistance to chemotherapy and to identify novel synergy between drug classes.
Study Rationale: This study will test ex vivo sensitivity to chemotherapies before and during treatment to test the hypotheses that 1) ex vivo sensitivity prior to standard chemotherapy correlates with subsequent clinical outcomes; 2) increased ex vivo resistance following initial exposure to chemotherapy provides greater correlation with early treatment failure and clinical outcomes; 3) whether in vivo chemotherapy exposure leads to changes in ex vivo drug sensitivity and 4) whether patterns of ex vivo drug sensitivity can identify novel drug combinations and predict clinical outcomes.
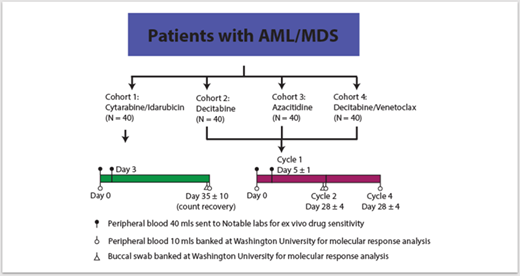
Study Design and Methods: This is a prospective, multi-arm, non-randomized single institution study enrolling subjects with AML and MDS who are anticipating treatment with one of four standard of care regimens (Figure 1).
Primary endpoint: Determine whether Day 0 ex vivo drug sensitivity, as measured by a normalized blast count score, correlates with clinical responses for all cohorts.
Key Secondary endpoints:
Determine whether the drug sensitivity score obtained for Day 0 ex vivo treatments for all cohorts correlates with molecular responses.
Determine whether the drug sensitivity score obtained for Day 0 ex vivo treatments for all cohorts correlates with survival.
Determine whether an increase in the drug sensitivity score for Day 3 ex vivo sensitivity correlates with reduced clinical outcomes.
Determine whether in vivo chemotherapy leads to increased ex vivo sensitivity to any class of drugs in more than 20% of patients treated on any study arm.
Determine whether decitabine and azacitidine are associated with overlapping or unique profiles in drug sensitivity changes on Day 5.
Determine whether ex vivo drug sensitivity correlates with the presence of clinically available mutations.
Key Inclusion Criteria:
Acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS)
Peripheral blood blasts > 1%
Peripheral white blood cell count > 1,000/μl.
Age ≥ 18 years
Anticipated treatment with any of the regimens in Figure 1
ECOG performance status ≤ 3
Key Exclusion Criteria
Prior chemotherapy with hypomethylating agents
Must not have received any chemotherapy within 7 days of enrollment, and any acute treatment-related toxicities must have returned to baseline. Patients may have received hydrea, but must discontinue at the time of enrollment. Prior TKI therapy is allowed, but must be discontinued within 3 days of baseline blood collection.
Currently receiving any other investigational agents.
Statistical Methods: Clinical responses for AML will be assessed according to the 2017 ELN AML Recommendations. For MDS, clinical responses will be assessed for response according to the 2006 IWG criteria. Descriptive statistics will be used to summarize baseline patient characteristics, therapies, clinical outcomes, and collection of biospecimens. Hierarchical clustering using Euclidean distance metrics and Ward minimum variance will be used to identify patient clusters with distinct ex vivo drug sensitivity patterns within a particular treatment cohort. For the primary endpoint, the correlation between clinical response and drug sensitivity will be assessed using the area under the receiver-operator curve (AUROC) and bootstrapping to test for significance. A generalized estimation equation model will be used to identify associations between mutations and ex vivo sensitivity to various drug classes within specific treatment cohorts.
Welch:Agios: Membership on an entity's Board of Directors or advisory committees; Janssen research: Research Funding; ArcherDx: Membership on an entity's Board of Directors or advisory committees; Notable labs: Research Funding. Richardson:Notable Labs: Current Employment, Current equity holder in private company. Kita:Notable Labs: Current Employment, Current equity holder in private company. Wen:Notable Labs: Current Employment, Current equity holder in private company. Tada:Notable Labs: Current Employment, Current equity holder in private company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal