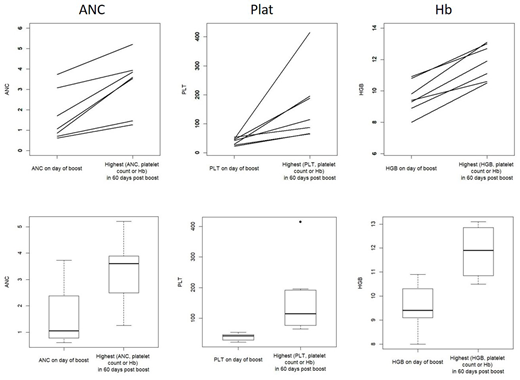
HLA-haploidentical donor transplants using T-replete grafts and posttransplant cyclophosphamide (HIDT) are increasingly utilized and have helped address the shortage of donors particularly among minority populations. While HIDT seem to produce similar survival outcomes to matched donor transplants, they may be subject to higher rates of early reactivation of some viruses. Myelosuppressive treatments for these viruses, other microbial infections and GVHD may produce prolonged periods of poor hematopoietic function and resulting cytopenia. Additional infusion of hematopoietic cells from the patient's donor that are ex-vivo depleted of T-cells, may help ameliorate these cytopenias and need for transfusions. Between June 2017 and June 2019 we performed 82 first HIDT at our center. Of these, seven patients (8.5%) underwent a T-cell depleted hematopoietic cell boost (HCB) following remobilization and collection of PBSC from the original donor in to correct refractory cytopenias. Patients were required to have >80% donor T-cell chimerism and have multilineage severe cytopenias for greater than three weeks after demonstrating prior engraftment. Active GVHD was not a contraindication to HCB. Patient characteristics were: Median age 69 (29-74); sex M4, F3; diagnoses - AML 3, NHL1, MPN 1, HL 1, SCD 1; prior autotransplant -2; regimen intensity of transplant - non-myeloablative -6, myeloablatve 1; median CD34 and CD3 doses of the original transplant were -5.01 (2.89-7.58) x 106/kg and 20.88 (3.7-41.6) x 107/kg respectively. All patients had 100% donor CD3 + cell and CD33+ cell chimerism in peripheral immediately prior to HCB. Median time between transplant and HCB was303 days (range 144-1048). Maximum grade acute GVHD and chronic GVHD pre-HCB were - gd 1(1), gd 2(3) gd 3(1) and severe chronic (1 patient). Four patients had active GVHD requiring systemic treatment at the time of HCB. Documented viral infections pre-HCB were: RTI- influenza (2) Parainfluenza(2), RSV(2) coronavirus(2) metapneumovirus(1) rhinovirus (1), adenovirus (1), HHV6 (1); Blood- CMV (3) adenovirus (3), HHV6 (1); Urine BKV (4). Original donors underwent repeat PBSC mobilization using G-CSF and leukapheresis targeting > 5 x 106 CD34 cells/kg. collection. The PBSC collection was CD34+ cell selected using a Miltenyi column (CliniMACS Plus CD34+ System) targeting < 1 x 105 CD3 cells/kg in the final product. No additional conditioning regimen was administered prior to HCB. Median doses infused for the HCB were CD34+ 4.89 x 106/kg (range 2.3-11.7) and CD3+ 0.21 x 105/kg (range 0.07-0.6). Median follow-up from day of HCB is 18.6m (13.2-37.2m). There were no infusional toxicities. One patient who had gd 1 aGVHD pre-HCB developed gd 3 aGVHD 4m post-HCB. However, this was felt to be related to withdrawal of immunosuppression. No other patient developed new GVHD or exacerbation of pre-existing GVHD. All patients demonstrated an increase in absolute neutrophil count (ANC) , platelet (plat) and hemoglobin (Hb) post HCB (Fig).Median values for maximal increase of ANC, plat and Hb from day of HCB to 60 days post HCB were 1.48 x 109/L, 73 x 109/L and 2.2 g/dL respectively (p<0.05 for all). All patients who were platelet and RBC transfusion dependent pre-HCB became transfusion independent within 60 days post-HCB. These data indicate that HCB using CD34+ cell selected re-mobilized PBSC collections from original haploidentical donor are safe and effective in correcting prolonged severe cytopenias following HIDT. Pre-existing GVHD and ongoing immunosuppressive therapy for GVHD are not a contraindication to their use
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal