
Background: Coronavirus disease 2019 (COVID-19), a multi-system disorder resulting from infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has affected 5.0 million individuals in the United States (US) resulting in more than 160,000 deaths. There is currently no proven effective therapy for SARS-CoV-2 infection beyond supportive care. Convalescent plasma (CP), collected from individuals who have recovered from SARS-CoV-2 infection, has been safely used to transfer virus-neutralizing antibodies to patients hospitalized with COVID-19. Herein we report on the clinical course and outcomes of patients who received CP for the treatment of COVID-19 across our health system.
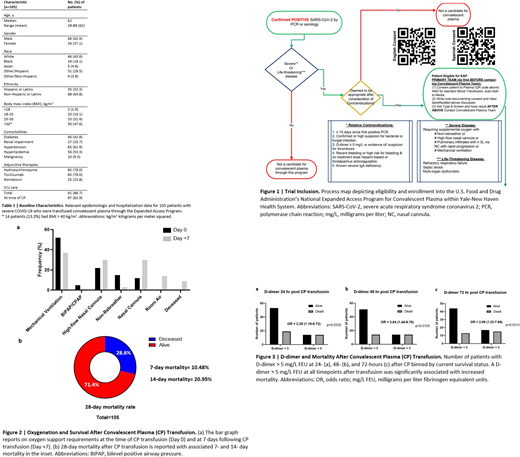
Methods: Hospitalized patients ≥ 18 years of age at 5 hospitals in the Yale-New Haven Health System with confirmed SARS-CoV-2 infection and severe or life-threatening disease (Figure 1) were enrolled in the US COVID-19 Expanded Access Program (EAP) and transfused 1 unit of CP. Patient outcomes were assessed at 7, 14, and 28 days after CP transfusion. Furthermore, we sought to determine mortality predictors in this patient cohort.
Results: 105 patients enrolled in the EAP were transfused CP from 4/12/2020 to 6/14/2020. Median age was 62 years (28-88 years). 62.9% of patients were male. Individuals of a non-white race comprised 56.2% of our cohort and 33.3% identified as Hispanic or Latinx. 47.6% of patients had a body mass index greater than 30, with 13.3% classified as extremely obese. Diabetes mellitus, hypertension, and hyperlipidemia were highly prevalent in our population. Concomitant therapy for COVID-19 included hydroxychloroquine (79.0%), tocilizumab (79.0%), and remdesivir (23.8%) (Table 1). 91 patients required the intensive care unit (ICU) during their hospital course, with 87 patients in the ICU at the time of CP transfusion. 42.9% of patients had an improvement in their World Health Organization (WHO) Ordinal Scale score by day 7 post-CP transfusion (median 4 days to improvement), while 9.5% demonstrated an increase in their WHO score indicating worsening oxygenation during the 7 days following CP (Figure 2). Mortality was 10.48% at 7 days, 20.95% at 14 days, and 28.57% at 28 days post-CP transfusion (Figure 2). Of the patients in the ICU at the time of CP, 56 (64.4%) de-escalated to non-ICU care after a median of 8 days from transfusion and 55 (63.2%) were ultimately discharged from the hospital. The median time from CP transfusion to discharge in survivors was 14 days (2-103 days), while median time from CP to death in non-survivors was 10 days (1-76 days). The mean time in days both from hospital admission to CP and from positive SARS-CoV-2 polymerase chain reaction (PCR) to CP trended slightly longer in non-survivors when compared to survivors (8.6 vs 6.9 days, p=0.218 and 9.7 vs 7.3 days, p=0.85, respectively). D-dimer levels >5 milligrams per liter fibrinogen equivalent units (mg/L FEU) were associated with increased mortality at 24 (OR 2.79, 95% CI 1.18-6.72), 48 (OR 3.64, 95% CI 1.44-9.70), and 72 hours (OR 2.99, 95% CI 1.23-7.66) post-CP transfusion (Figure 3). Twelve patients (11.4%) on prophylactic or intermediate dose anticoagulation were subsequently escalated to therapeutic dosing during the 7 days after CP transfusion. Furthermore, a ferritin level of >3000 nanograms per milliliter (ng/mL) on the day of CP was associated with increased mortality (OR 5.14, 95% CI 1.34-19.68).
Conclusions: CP therapy was administered through the EAP to COVID-19 patients with severe disease and with advanced age, high frequency of obesity, and extensive co-morbidity. In this COVID-19 population with high expected mortality, 42.9% of patients improved by WHO Ordinal Scale score within 7 days of CP transfusion and 52.4% were alive and discharged at 28 days. Baseline ferritin and d-dimer levels at 24, 48, and 72 hours post-CP were predictors of mortality, the latter raising the possibility that the increased thrombotic risk associated with COVID-19 may be exacerbated by administration of blood products from donors potentially in a residual procoagulant state. Further studies by our group are underway to assess hemostatic balance in donor CP, to estimate associations with outcomes by comparing patients who received CP with a matched control cohort of COVID-19 patients who did not receive CP, and to evaluate efficacy of CP in a randomized, placebo-controlled clinical trial.
McLeod:Gilead Pharmaceuticals: Other: Medical Advisor .
We have described in this abstract patients across our health system who received investigational convalescent plasma therapy through enrollment in the "Expanded Access to Convalescent Plasma for the Treatment of Patients with COVID-19" protocol that is funded by BARDA and run by the Mayo Clinic, where primary IRB protocol is held. Previous guidance issued by the FDA regarding investigational use of COVID-19 convalescent plasma included recommendations for the expanded access program as a method by which to facilitate access to this blood product across the nation. Safety data reported thus far from the expanded access program has demonstrated no concerning findings, with a very low rate of serious adverse events. Therefore given the overall tolerability of convalescent plasma and the lack of other proven therapies for COVID-19, we believe it is important to report these findings even in the absence of current approval for convalescent plasma transfusion in the management of COVID-19.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal