Introduction: Tyrosine kinase inhibitors (TKIs) are the standard-of-care for patients with chronic myeloid leukemia in chronic phase (CML-CP) and are associated with improved outcomes. The risk of cardiovascular (CV) events has emerged as an important consideration during TKI therapy, mostly due to associated complications and the need to understand causality and proper mitigation. While nilotinib has been associated with an increased risk of CV events, few prospective studies have assessed the CV and metabolic risk profile of TKIs administered during routine clinical practice in a real-world setting. Importantly, data regarding the role of baseline CV risk factors at initiation of specific TKIs and subsequent CV events are limited. Here we assess CV and metabolic risk in patients with CML-CP undergoing first-line treatment with TKIs in a real-world setting.
Methods: CA180-653 (NCT03045120) is an ongoing, non-interventional, prospective clinical trial characterizing the impact of approved TKIs (bosutinib, dasatinib, imatinib, and nilotinib) on CV and metabolic risk factors following initial TKI therapy in newly diagnosed patients with CML-CP in the USA. Baseline clinical and demographic characteristics, including medical history, vital signs, and evidence of additional comorbid conditions were assessed. CV and metabolic risk factors, as well as CV disease surrogates, were also measured, including ankle brachial index (ABI), echocardiogram (ECHO), electrocardiogram (EKG), and Framingham coronary heart disease score. Metabolic risk variables included fasting blood glucose, HbA1c, and fasting lipid panel. Enrolled patients were analyzed at both baseline and at six months after study enrollment.
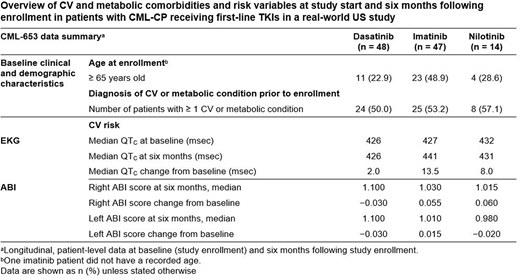
Results: Between March 2017 and December 2019, 109 patients were enrolled at 16 study sites across the USA. The analysis included patients treated with dasatinib (n = 48), imatinib (n = 47), and nilotinib (n = 14); key characteristics and CV findings are summarized in the Table. In all, 48.9% of patients prescribed imatinib were ≥ 65 years of age, compared with 22.9% of dasatinib and 28.6% of nilotinib patients. Patients treated with dasatinib had a marginally lower proportion of reported baseline CV/metabolic conditions (50.0%) compared to imatinib (53.2%) and nilotinib (57.1%). Interestingly, among patients with baseline Ca2+ scoring, 57.1% of nilotinib patients had coronary artery calcification present at baseline compared to 35.7% of imatinib patients and 28.9% of dasatinib patients. Most patients receiving an ECHO (96%) or EKG (99%) were assessed as normal or presenting clinically not significant abnormalities both at baseline and at the 6-month follow-up. Baseline corrected QT (QTC) scores were similar for dasatinib, imatinib, and nilotinib patients. Among patients with a change in QTC at six months, patients on imatinib had a larger change in median score (13.5 msec) than patients on nilotinib (8.0 msec) or dasatinib (2.0 msec). At six months, changes in ABI scores were small and unlikely to be statistically significant: left ABI scores changed by -0.030, -0.020, and 0.015 for patients on dasatinib, nilotinib, and imatinib respectively; right ABI scores changed by -0.030, 0.055, and 0.060 for patients on dasatinib, imatinib, and nilotinib, respectively. Additional longitudinal data will be presented.
Conclusions: These preliminary findings confirm that just over half of patients with CML-CP in the USA have CV/metabolic comorbidities present at baseline, as measured by reproducible and sequentially evaluable studies known to be predictive of systemic vascular disease risk. Measurement of baseline clinical data is vital for assessing CV and metabolic risk in the US oncology settings. CA180-653 was powered to capture the impact of first- and second-generation TKIs on CV and metabolic risk factor outcomes within treatment arms, rather than between treatment arms. Further analysis is ongoing to determine the differential effects of TKIs used in CML-CP, the effect of long-term TKI therapy, and the value of specific CV evaluations to assess optimally and manage risk in patients with CML-CP.
Study support:BMS.
Mauro:Sun Pharma/SPARC:Research Funding;Pfizer:Consultancy, Honoraria, Other: Travel, Accommodation, Expenses, Research Funding;Takeda:Consultancy, Honoraria, Other: Travel, Accommodation, Expenses, Research Funding;Novartis:Consultancy, Honoraria, Other: Travel, Accommodation, Expenses, Research Funding;Bristol-Myers Squibb:Consultancy, Honoraria, Other: Travel, Accommodation, Expenses, Research Funding.Oehler:Pfizer:Research Funding;Bristol-Myers Squibb, Takeda:Consultancy.McCloskey:Jazz:Consultancy, Honoraria;AbbVie:Consultancy, Honoraria;Takeda:Consultancy, Honoraria;BMS:Consultancy, Honoraria;Amgen:Consultancy, Honoraria.Heinrich:Novartis:Consultancy, Patents & Royalties: Patent on treatment of GIST licensed to Novartis;Blueprint Medicines:Consultancy;Deciphera:Consultancy, Speakers Bureau.DeGutis:Bristol-Myers Squibb:Current Employment, Current equity holder in publicly-traded company.Tabano:Bristol-Myers Squibb:Current Employment.Khan:Bristol-Myers Squibb:Current Employment, Current equity holder in publicly-traded company.Moslehi:AstraZeneca, Janssen, BMS, Boston Biomedical, Immunocure, Myovant, Boston Biomedical, Deciphera:Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal