Background:
Chimeric antigen receptor T-cell (CAR T) immunotherapy is an evolving treatment for relapsed/ refractory non-Hodgkin lymphoma (NHL) and multiple myeloma (MM). There is a growing need to elucidate the infectious complications of BCMA- and CD19-directed CAR T therapy. We performed a single-center retrospective analysis of infection outcomes up to 1-year post BCMA and CD19-directed CAR T treatment.
Methods:
All patients treated at our institution with a BCMA-directed CAR T therapy for MM or with a CD19-directed CAR T for NHL from 2018-2020 were analyzed for risk factors for infection and infectious complications. Bacterial, viral and fungal infections were recorded if there was a microbiologic or histopathologic diagnosis or if clinical suspicion for infection required empiric treatment. Infection severity was classified as mild, moderate, severe, life-threatening, or fatal as previously described (Young et al. 2016, van Burnik et al. 2007). Infections were identified from the day of the first CAR T-cell infusion up to 1 year after infusion. Observation of infections was terminated at the time of disease progression, initiation of next therapy, or death, whichever occurred first. Fisher's exact test and Wilcoxon rank-sum test were used to compare between cohorts. Poisson mixed effects model with a subject-specific random intercept and an offset to account for the duration at risk was used to identify risk factors for infections.
Results:
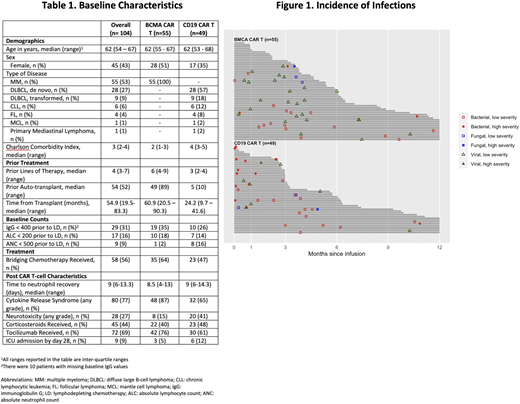
Of the 104 subjects in this study, 55 patients (53%) had MM treated with BCMA CAR T and 49 patients (47%) had NHL treated with CD19 CAR T. Median number of prior therapies was 6 (4 - 9) in the BCMA cohort and 3 (2-4) in the CD19 cohort (Table 1). Prior to starting lymphodepleting (LD) chemotherapy, most patients did not have IgG< 400, ALC< 200, or ANC< 500. Almost all the patients were on antibacterial (99%), antiviral (99%) and antifungal (92%) prophylaxis (ppx), with 18%, 90% and 9% of patients starting this before LD chemotherapy, respectively. Median follow-up time was 5.8 months (95% CI: 4.2-6.4).
In total, there were 87 infection events (48 bacterial, 33 viral, and 6 fungal) observed in 56 patients (54%), with 47 infections in 29 (53%) patients in the BCMA CAR T cohort and 40 infections in 27 (55%) patients in the CD19 CAR T cohort (p =0.9). The BCMA cohort had 19 bacterial (40%) vs 29 bacterial (73%) in CD19 cohort (p=0.005), while BCMA cohort had 25 viral (53%) vs 8 viral (20%) in CD19 cohort (p=0.002). Fungal infection rates were comparable between BCMA and CD19 cohorts, 3 (6%) vs 3 (8%) respectively (p=1). Among the infections that occurred, 20 (23%) were high severity occurring in 16 patients (15%) of the overall cohort. Four high severity infections (5%) occurred in 3 patients (5%) in the BCMA cohort while 16 high severity infections (18%) occurred in 13 patients (27%) in the CD19 cohort (p < 0.001) (Figure 1). The BCMA cohort had higher rates of respiratory infections (68% vs 50%, p=0.1), while the CD19 cohort had higher rates of bloodstream infections (15% vs 2%, p=0.05) and gastrointestinal infections (10% vs 0%, p=0.04). The rates of grade (Gr) 3-4 neutropenia and IgG < 300 in both the cohorts at various time points post CAR T were comparable. At 9-12 months, Gr 3-4 neutropenia was 7% vs 8% (p=1) and IgG < 300 was 7% vs 33% (p=0.1) for the BCMA and CD19 cohorts respectively. Adjusting for time periods, risk factors for development of infections were use of steroids (incidence rate ratio [IRR] 1.6, 95% CI: 1.1-2.5, p=0.03) and post CAR T hypogammaglobulinemia (IgG < 600) (IRR =2.1, 95% CI: 1.2-3.9, p=0.02).
Conclusions:
This retrospective study is one of the largest studies to date comparing the post CAR T infections rates between BCMA and CD19 directed CAR T treated patients. While the incidence of infection, use of antimicrobial ppx, and rates of Gr 3-4 neutropenia and hypogammaglobulinemia were comparable between BCMA and CD19 CAR T cohorts, viral infections were more common post BCMA CAR T while bacterial infections were more frequent post CD19 CAR T. Use of steroids as well as post CAR T hypogammaglobulinemia are possible risk factors for development of infections. Further studies are needed to examine the infectious complications post-CAR T treatment, characterize the underlying risk factors, and to establish appropriate prophylactic approaches in patients undergoing CD19- and BCMA-directed CAR T therapy.
Fakhri:University of California San Francisco: Current Employment. Ai:Nurix Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding; ADC Therapeutics, Kymera: Membership on an entity's Board of Directors or advisory committees. Martin:Seattle Genetics: Research Funding; GSK: Consultancy; Sanofi: Research Funding; AMGEN: Research Funding; Janssen: Research Funding. Wolf:Adaptive: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Shah:BMS, Janssen, Bluebird Bio, Sutro Biopharma, Teneobio, Poseida, Nektar: Research Funding; GSK, Amgen, Indapta Therapeutics, Sanofi, BMS, CareDx, Kite, Karyopharm: Consultancy. Andreadis:Genentech: Other: Spouse Employee (salary and stock); Novartis: Research Funding; Celgene/Juno: Research Funding; Amgen: Research Funding; Merck: Research Funding; Gilead/Kite: Other: Advisor; Jazz Pharmaceuticals: Other: Advisor; Astellas: Other: Advisor; Seattle Genetics: Other: Advisor; Karyopharm: Other: Advisor; Incyte: Other. Wong:GSK: Research Funding; Amgen: Consultancy; Sanofi: Membership on an entity's Board of Directors or advisory committees; Bristol Myers Squibb: Research Funding; Roche: Research Funding; Janssen: Research Funding; Fortis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal