Background:
Allogeneic hematopoietic stem cell transplantation (HCT) is a potentially curative procedure for a variety of hematologic malignancies. However, relapse disease and graft-versus-host disease (GVHD) remain to be the main obstacle for a successful HCT. Thus, adequate immune suppression to minimize the risk of high-grade GVHD while not over suppression of donor immunity to allow graft versus tumor effect is crucial.
Matched unrelated donor transplant has a higher rate of GVHD as compared to matched sibling donor transplant due to minor histocompatibility mismatch. Rabbit antithymocyte globulin (ATG), a polyclonal antibody produced by immunizing rabbits with human thymocytes, has been utilized as prophylaxis against GVHD.
ATG dosing by weight has been the standard. Recent pharmacokinetic (PK) studies revealed that ATG levels and clearance vary significantly among patients receiving weight-based dosing of ATG. Recipient lymphocyte count before receiving ATG has been described as a modulator of both ATG PK and clinical outcomes after ATG-conditioned HCT.
The Parachute-Study utilizing an individualized ATG dosing approach has shown more rapid immune reconstitution without affecting the incidence of acute GVHD and graft failure. In this study, we are comparing the outcomes of individualized dosing of ATG versus weight-based dosing.
Method:
This is a single institutional study carried out at the Bone Marrow Transplant Program at the University of Oklahoma Health Science Center. It was started as a case-control cohort study in July 2018 when individualized dosing of ATG was initiated, and continues as a historically controlled non-randomized prospective clinical study investigating individualized versus weight-based dosing of ATG.
Subjects over 18 years of age who are undergoing matched unrelated donor (MUD) stem cell transplant, with myeloablative or reduced-intensity conditioning, peripheral blood or bone marrow stem cell source, for myeloid or lymphoid malignancies were included in the study. We excluded subjects with HLA mismatch or sibling donors.
Individualized dosing was based on the previously validated PK model with cumulative doses varying between 2 to 10 mg/kg, based on weight, recipient lymphocyte counts before the first dose of ATG, and stem cell source, starting day -9; while the standard weight-based dosing of ATG is 4 mg/kg divided into 3 days pre-transplant.
The study endpoints are to evaluate the difference between treatment groups on (1) GVHD and its severity; (2) relapse-free survival (RFS) and (3) overall survival (OS).
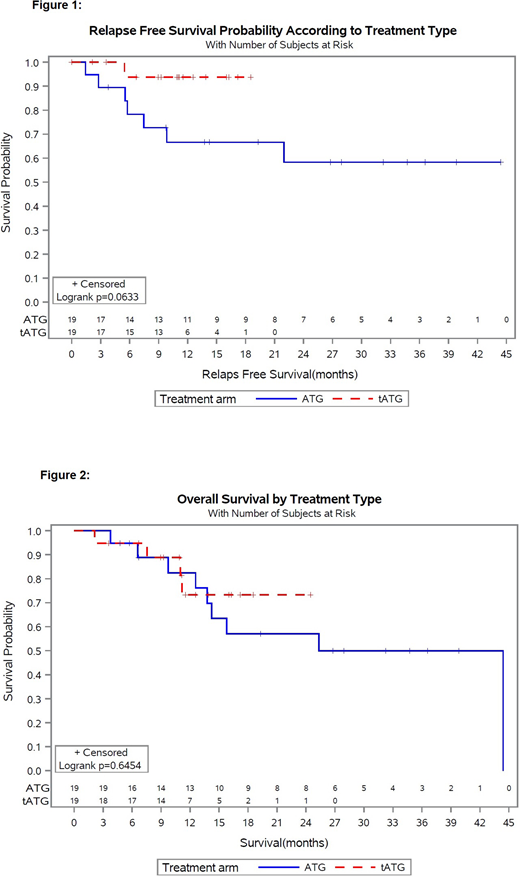
Univariate logistic regression analysis was used to evaluate the probabilities of GVHD in both treatment arms. Multivariable analysis was done to adjust for all covariates between study arms using adjusted logistic. OS and RFS were computed using the Kaplan-Meier curves.
Results:
The study included 38 subjects undergoing MUD HCT for myeloid or lymphoid malignancies. Subjects included are in 2 cohorts, 19 subjects in the intervention arm using individualized targeted ATG (tATG group), and 19 subjects in the matched control arm using weight-based dosing ATG (ATG group).
In a univariate unadjusted logistic regression analysis, the risk of developing GVHD is numerically higher in the ATG group than in the tATG group (OR=1.339, p=0.70). However, the proportion of acute GVHD is significantly higher in the tATG group than the ATG group (73.68% vs 31.58%, p=0.022). Also, the proportion of higher grade acute GVHD is significantly higher in the tATG group than the ATG group (31.58% vs 0%, p=0.020).
RFS is longer in the tATG group than the ATG group, tending statistical significance (p=0.063). However, there is no difference in OS between study arms (p=0.645). [Figures 1 and 2]
In a multivariable-adjusted logistic regression, adjusting for age at HCT, diagnosis, disease status at HCT, prior lines of therapy, and stem cell source, no confounder was found to be significantly associated with GVHD.
Conclusion:
Individualized targeted dosing of ATG (tATG), based on weight, recipient lymphocyte counts and stem cell source, increases the risk of acute GVHD when compared to standard fixed-dosing method, however, it improves RFS, implying possibly better immune reconstitution providing improved graft versus leukemia effect.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal