Background
Follicular lymphoma (FL) is the second most common type of non-Hodgkin lymphoma (NHL) and most common of the clinically indolent NHLs. Although often considered an incurable disease, overall survival has increased significantly with refinement in diagnostic techniques and the addition of rituximab. The course of FL is quite variable and presence of symptoms, organ dysfunction, cytopenias, aggressiveness of tumor are all taken into consideration when deciding individual treatment. In this study, we evaluated a large patient cohort with FL treated over a 35 year period for progression free survival (PFS), overall survival (OS) based on FLIPI score, tumor grade, and treatment regimen and also looked at causes of late failures.
Methods
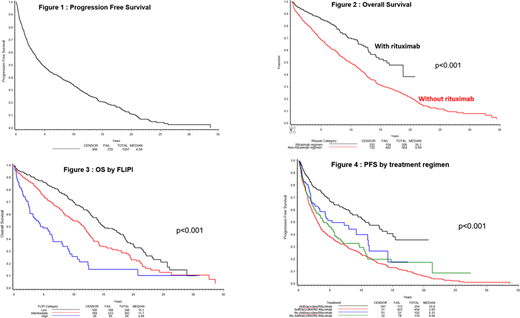
We evaluated 1037 patients (pts) from the Nebraska Lymphoma Study Group that were diagnosed with FL between the years of 1983-2020. Descriptive statistics were stratified according to age, histological subtype, treatment regimen, FLIPI category, presence and type of secondary malignancy. PFS was calculated from the time of diagnosis to progression or death and OS was the time from diagnosis to death from any cause. PFS and OS were plotted as Kaplan-Meier curves with statistically significant p<0.05.
Results
The median age at diagnosis and treatment was 61 years (yrs, range 17-91). A total of 9.1% were characterized as FLIPI high risk, 37.8% intermediate risk, and 33.6% low risk, 19.5% unavailable. Among the histological grade, 23.1% had FL- grade 1, 30.2% FL-2, 27.3% FL-3A, 2.5 % FL-3B and 16.9 % Composite Lymphoma. Anthracycline + rituximab was given in 24.5% of pts, whereas 43.8% of pts received an anthracycline based regimen without rituximab, 9.8% received rituximab without an anthracycline and 10.6% received neither of these agents. 6.75% (70 pts) were later found to have secondary malignancies of which 11 pts had myelodysplastic syndrome, 10 pts had acute leukemia and 9 pts had lung cancer. With a median follow up of 9.2 yrs and a maximum of 36 yrs, 29.7% (308 pts) had not relapsed.
The median PFS across all groups was 4.6 yrs (Fig 1) and OS was 12.1 yrs. Median OS was significantly longer in patients that received rituximab at 16.1 yrs as compared to patients that did not receive rituximab at 9.89 yrs (Fig 2). PFS was 8.6 yrs, 3.6 yrs and 2.1 yrs and OS was 15.1 yrs, 11.7 yrs and 4.9 yrs in FLIPI low, intermediate and high risk groups respectively (p=<0.001) (Fig 3), suggesting that survival was influenced by FLIPI score. Median PFS in FL-3B and FL-3A was 9.2 yrs and 5.2 yrs respectively which is longer than 4.7 yrs and 4.2 yrs for FL-1 and FL-2 (p=0.24). OS in FL-3A and FL-3B subgroups was 10.8 yrs while it was 11.6 yrs and 14.3 yrs in FL-2 and FL-1 (P=0.081). PFS is significantly longer at 10.6 yrs in pts treated with both anthracycline and rituximab containing regimen as compared to 5.3 yrs in pts treated with rituximab alone and 3.05 yrs in pts that had only anthracycline based regimen (p=<0.001) (Fig 4). The median OS also was significantly higher in the combination regimen group at 18.8 yrs as compared to 11.3 yrs in rituximab only group and 9 yrs in anthracycline based regimen group (p=<0.001).
When pts with FL-3A and FL-3B were grouped together and stratified according to treatment regimen, the group that received anthracycline and rituximab combination has highest PFS and OS at 13.3 yrs and 18.8 yrs (p<0.001). when pts with FL-3A were analyzed separately and stratified by treatment regimen, the results of PFS and OS were similar and statistically significant. However, of the 24 pts in FL-3B group, analysis revealed that PFS and OS was longer in anthracycline based regimen only group, however results were not statistically significant.
Among the pts that relapsed/died after 10 years (n=190), the cause of death was relapsed lymphoma in 13.7%, unknown in 55.8%, secondary malignancies in 4.2%, treatment related in 2.6% and not related to disease in 23.7%. A total of 278 pts survived > 10 yrs, and of these pts, 119 (30%) had not relapsed at the last follow up.
Conclusion
The addition of rituximab to standard anthracycline based chemotherapy has resulted in significant improvements in the PFS and OS rates of FL. These results also support the prognostic value of the FLIPI in patients treated in the rituximab era. Late relapses after 10 yrs from disease can occur, but 11.5% of patients had not relapsed with long term follow up. Secondary malignancies are also an important consideration in the long term survivors.
Lunning:Acrotech: Consultancy; TG Therapeutics: Research Funding; Novartis: Consultancy, Honoraria; Kite: Consultancy, Honoraria; Karyopharm: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Gilead: Consultancy, Honoraria; Curis: Research Funding; Beigene: Consultancy, Honoraria; Aeratech: Consultancy, Honoraria; Bristol Meyers Squibb: Consultancy, Honoraria, Research Funding; AstraZeneca: Consultancy, Honoraria; Legend: Consultancy; Verastem: Consultancy, Honoraria; ADC Therapeutics: Consultancy. Armitage:Trovagene/Cardiff Oncology: Membership on an entity's Board of Directors or advisory committees; Samus Therapeutics: Consultancy; Ascentage: Consultancy. Vose:Bristol-Myers Squibb: Research Funding; Karyopharm Therapeutics: Consultancy, Honoraria; Seattle Genetics: Research Funding; Allogene: Honoraria; AstraZeneca: Consultancy, Honoraria, Research Funding; Kite, a Gilead Company: Honoraria, Research Funding; Wugen: Honoraria; Novartis: Research Funding; Celgene: Honoraria; Incyte: Research Funding; Roche/Genetech: Consultancy, Honoraria, Other; Verastem: Consultancy, Honoraria; Miltenyi Biotec: Honoraria; Loxo: Consultancy, Honoraria, Research Funding; Janssen: Honoraria; Epizyme: Honoraria, Research Funding; AbbVie: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal