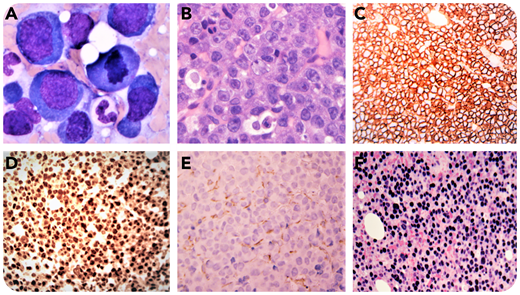
A 67-year-old HIV-negative man presented with a history of sinus lesions and elevated serum monoclonal immunoglobulin G kappa but no evidence of lytic bone lesions. Serum calcium, creatinine, and complete blood count were normal. Peripheral blood smear was unremarkable. A bone marrow workup showed normocellularity with trilineage hematopoiesis and partial involvement by an abnormal population of large cells that exhibited amphophilic cytoplasm, oval nuclei, and variably prominent nucleoli (panel A: Wright-Giemsa stain, original magnification ×1000; panel B: hematoxylin and eosin stain, original magnification ×400). By immunohistochemistry, these abnormal cells were positive for CD138 (panel C; original magnification ×200), MUM1 (panel D; original magnification ×200), CD56, C-MYC with kappa restriction, negative for PAX5 (panel E; original magnification ×200), CD20, CD45, CD30, CD117, cyclin D1, BCL-2, BCL-6, HHV8, and ALK1. Epstein-Barr (virus)–encoded RNAs (EBERs) were positive by in situ hybridization (panel F; original magnification ×200). The proliferation index by Ki-67 immunostaining approached 95%. C-MYC translocation was demonstrated by fluorescence in situ hybridization (FISH), but no other myeloma-associated chromosomal abnormalities were detected by FISH. A diagnosis of plasmablastic lymphoma (PBL) was rendered. Similar features were seen in his sinus mass.
PBL and plasmablastic myeloma are rare yet aggressive hematologic neoplasms, with identical morphologic features and immunophenotypical profiles, which often cause diagnostic challenges. The presence of EBER positivity and absence of myeloma abnormalities detectable by FISH as well as absence of myeloma-defining signs of hypercalcemia, renal failure, anemia, and bone disease (CRAB) in this patient, support the diagnosis of PBL.
A 67-year-old HIV-negative man presented with a history of sinus lesions and elevated serum monoclonal immunoglobulin G kappa but no evidence of lytic bone lesions. Serum calcium, creatinine, and complete blood count were normal. Peripheral blood smear was unremarkable. A bone marrow workup showed normocellularity with trilineage hematopoiesis and partial involvement by an abnormal population of large cells that exhibited amphophilic cytoplasm, oval nuclei, and variably prominent nucleoli (panel A: Wright-Giemsa stain, original magnification ×1000; panel B: hematoxylin and eosin stain, original magnification ×400). By immunohistochemistry, these abnormal cells were positive for CD138 (panel C; original magnification ×200), MUM1 (panel D; original magnification ×200), CD56, C-MYC with kappa restriction, negative for PAX5 (panel E; original magnification ×200), CD20, CD45, CD30, CD117, cyclin D1, BCL-2, BCL-6, HHV8, and ALK1. Epstein-Barr (virus)–encoded RNAs (EBERs) were positive by in situ hybridization (panel F; original magnification ×200). The proliferation index by Ki-67 immunostaining approached 95%. C-MYC translocation was demonstrated by fluorescence in situ hybridization (FISH), but no other myeloma-associated chromosomal abnormalities were detected by FISH. A diagnosis of plasmablastic lymphoma (PBL) was rendered. Similar features were seen in his sinus mass.
PBL and plasmablastic myeloma are rare yet aggressive hematologic neoplasms, with identical morphologic features and immunophenotypical profiles, which often cause diagnostic challenges. The presence of EBER positivity and absence of myeloma abnormalities detectable by FISH as well as absence of myeloma-defining signs of hypercalcemia, renal failure, anemia, and bone disease (CRAB) in this patient, support the diagnosis of PBL.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal