Abstract
Introduction: Bleeding is a serious complication among neonates undergoing cardiopulmonary bypass (CPB) and it is linked to significant morbidity and mortality. Current standard of care treatment for bleeding after CPB focuses on the transfusion of adult blood products, including platelets and cryoprecipitate. However, prior work by Nellenbach et al. has demonstrated structural differences between neonatal and adult clotting components. Importantly, neonatal and adult fibrin do not fully integrate during clot formation which may contribute to ineffective clot formation and/or increased thrombotic risk following transfusion of adult cryoprecipitate to neonates. There has been increased interest in using human fibrinogen concentrate (HFC) in treating bleeding in the post-CPB neonate; however, HFC has not been validated in this population through evidence-based means. This study analyzed structural and degradation properties of post-CPB clots +/- the ex vivo addition of HFC and compared structural and degradation properties of post-CPB clots after the in vivo transfusion of HFC versus cryoprecipitate.
Methods: Human neonatal plasma samples were collected from patients undergoing CPB at the Children's Hospital of Atlanta. For ex vivo studies, samples were taken at baseline, post-bypass, and post-transfusion of cryoprecipitate (n = 18 patients). Clots were formed for analysis from samples alone as well as post-bypass samples with the addition of 0.5 or 0.9 mg/mL HFC (RiaSTAP, CSL Behring) and structure was examined through confocal microscopy. Clot degradation was assessed through a microfluidic fibrinolysis assay. For in vivo studies, samples were taken at baseline, post-transfusion of cryoprecipitate or HFC, upon ICU arrival, and at 24 hours post-surgery (n = 36 patients). Clots were formed from samples and structure was examined through confocal microscopy. Clot degradation was assessed through a plate-based fibrinolysis assay.
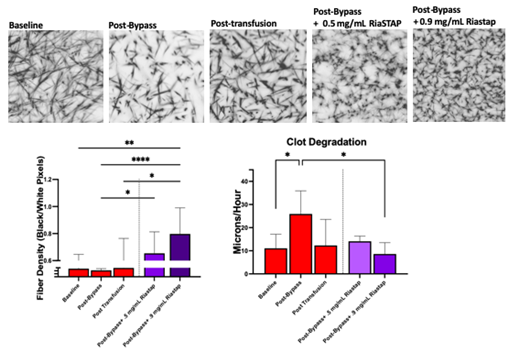
Results: In ex vivo studies, clot structural analysis demonstrated no significant differences in fiber density between samples collected at different time points (baseline = 0.541 ± 0.105, post-bypass = 0.431 ± 0.111, post-transfusion = 0.594 ± 0.170). The addition of 0.5 mg/mL or 0.9 mg/mL HFC to post-bypass samples led to a significant increase in fiber density (0.5 mg/mL HFC=0.654 ± 0.158, p=0.02; 0.9 mg/mL HFC= 0.797 ± 0.193, p<0.0001). Functional microfluidic analysis of clot degradation demonstrated significantly faster degradation times among post-bypass samples when compared to baseline samples (baseline degradation rate = 11.061 ± 6.087, post-bypass degradation rate = 25.906 ± 9.990 microns/hour, p=0.04). The addition of 0.5 mg/mL HFC resulted in a slower degradation rate from the original post-CPB degradation rate, but did not reach statistical significance (0.5 mg/mL HFC=14.091 ± 2.241, p=0.14). However, the addition of 0.9 mg/mL HFC resulted in a significantly slower degradation rate (0.9 mg/mL HFC=8.594 ± 6.087, p=0.01). Studies comparing in vivo transfusion of cryoprecipitate and HFC demonstrated no significant difference between treatment groups in clot density or degradation rate for any sample time point.
Conclusion: We identify patterns in structural properties of clots formed after the transfusion of HFC that are consistent with successful hemostasis. However, caution is warranted regarding potentially thrombotic risks and should be carefully analyzed in future studies.
Figure: Effect of Ex Vivo HFC Addition on Clot Structure and Degradation. (A) Representative confocal imaging of clots formed from different samples and HFC dosages (scale = 50 um). (B) Effect of HFC Addition on Clot Fiber Density. Addition of both 0.5 and 0.9 mg/mL HFC dosages to post-bypass sample result in statistically significant increases in fiber density compared to post-bypass samples. (C) Effect of HFC Addition on Clot Degradation Profiles. Addition of 0.9 mg/mL HFC to post-bypass sample leads to statistically significant slower fibrinolysis.
Brown: Selsym Biotech, Inc.: Other: Co-Founder and CEO.
RiaSTAP (human fibrinogen concentrate) is FDA approved for the treatment of congenital hypofibrinogenemia.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal