Abstract
Background: Gemtuzumab (GO) is an antibody drug conjugate that links a CD33 antibody to calicheamicin, a potent DNA-damaging agent. GO has been studied in combination with standard chemotherapy in multiple randomized clinical trials, though the doses and schedules of GO in these studies varied significantly. In a meta-analysis, 1 the addition of GO was found to improve relapse-free (RFS) and overall survival (OS), particularly in patients with favorable cytogenetics. It is now approved for use in combination with 7+3 in newly diagnosed CD33-positive AML. The studies that supported its approval were heterogenous and, in clinical practice, the uptake and utilization patterns for GO have been wide-ranging. At Johns Hopkins Sidney Kimmel Cancer Center, a single dose of GO at a dose of 3 mg/m2 has been incorporated into standard 7+3 induction for patients with core binding factor (CBF) AML since . Herein, we report the impact of this practice change on clinical outcomes for patients with CBF AML.
Methods: 72 patients with newly-diagnosed, previously untreated CBF AML from 2008-2020 were identified. Electronic medical records were reviewed for initial CBF AML presentation, management, and outcomes. Patient, disease, and transplant characteristics were summarized by treatment groups using descriptive statistics. Group differences were tested via Wilcoxon rank-sum test, chi-square test of independence, and Fisher's exact disease. Kaplan-Meier estimates were reported for OS and RFS. Group differences were tested via log-rank test. All analyses were carried out with R version 4.0.2 using the "survival" and "cmprsk" packages (R Foundation for Statistical Computing, Vienna, Austria).
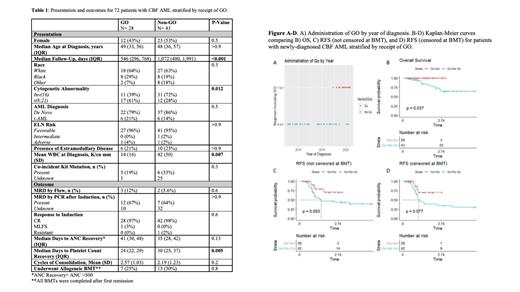
Results: There were 28 (40%) patients who received GO and 43 (60%) who did not (non-GO) (Table 1). The percentage of patients in the GO group who had favorable ELN risk was similar to the non-GO group (p>0.9). The proportion of patients with inv(16) was lower in the GO group (p=0.018) while the proportion of patients with t(8;21) was greater in the GO group (p=0.018). At presentation, the GO group had a significantly lower mean WBC compared to the non-GO group (p = .007). The rates of complete response (CR) after induction were similar between the GO and non-GO groups (p = 0.6). The GO group took longer to achieve neutrophil count (0.5 K/cu mm) recovery (p=0.13) whereas the non-GO group took longer to achieve a platelet count of 100K/cu mm (p=0.005). The rates of post-induction measurable residual disease (MRD) by flow cytometry were similar between the GO and non-GO groups (p=0.6). 7 (24%) patients in the GO group and 13 (30%) of patients in the non-GO group underwent allogeneic bone marrow transplant in first remission. The only non-hematologic adverse effects noted in the GO group were rapid weight gain in 2 patients (7%) and grade I/II elevated liver enzymes in 5 patients (18%). No grade III-IV liver enzyme abnormalities. There were no therapy-related deaths in the GO group and no episodes of vaso-occlusive disease in those who went on to transplant. There was a trend towards improved RFS (p=0.05, Figure C-D) and significantly improved OS (p=0.04, Figure B) favoring patients who received a one-time dose of GO.
Conclusions: Patients who received GO had a trend towards improved RFS and significantly improved OS compared to patients who did not. This real-world study suggests that there may be a benefit, with little detriment, to the addition of a single dose of GO. The study, however, is limited by differences between the two groups including WBC at presentation, distribution of inv(16) vs. t(8;21), the eras in which patients were diagnosed and treated, and shorter median follow-up time for the GO group. Our study was further limited by missing data for a significant proportion of patients with regards to C-KIT and rates of post-induction MRD by PCR. It is important to note that this study compared GO and any regimen (not limited to 7+3) to any regimen without GO. Treatment protocols evolved during GO utilization and these changes in practice patterns could have impacted clinical outcomes. Lastly, this study highlights the fact that patients with CBF AML can expect to have favorable outcomes.
References:
1. Hills RK, et al. Addition of gemtuzumab ozogamicin to induction chemotherapy in adult patients with acute myeloid leukaemia: A meta-analysis of individual patient data from randomised controlled trials. Lancet Oncol. 2014;15(9):986-996.
DeZern: Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Taiho: Consultancy, Membership on an entity's Board of Directors or advisory committees; Bristol-Myers Squibb: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal