Abstract
Introduction
Allogeneic Hematopoietic Cell Transplantation (allo-HCT) has proved its efficiency in reducing Acute Myeloid Leukemia (AML) recurrence, although it was associated with high rates of complications especially in older patients. The worldwide number of allo-HCT has increased within 35 years, from 10.000 transplantations before 1985 to over a million in 2012. The decision to perform transplantation depends on the estimated risk-benefit ratio. High-risk prognostic factors include cytogenetics, age at diagnosis, presence of comorbidities and the response to treatment. By using combination of risk factors, international recommendations have been published to harmonize AML care and maximize the benefit of using allo-HCT. The principal aim of this study is to describe real life AML care management in all consecutive patients diagnosed and registered on 3 regional cancer registries in France, to analyze their outcome after different therapeutic strategies, following or not the international recommendations.
Method
This retrospective study included all AML patients diagnosed between January 2012 and December 2016 reported to the French population data-based of regional cancer registries specialized in hematological malignancies. Allo-HCT data were extracted from the Société Française de Greffe de Moelle et de Thérapie Cellulaire (SFGM-TC) registry. Two groups of patients were defined according to the treatment received: i) group 1, patients who have received the best recommended care including allo-HCT considering HLA compatibility and best donor choice or best conventional treatment according to therapeutic guidelines based on individuals and clinical characteristics from The American Society for Blood and Marrow Transplantation guidance; ii) group 2, patients who received a treatment outside the recommendations.
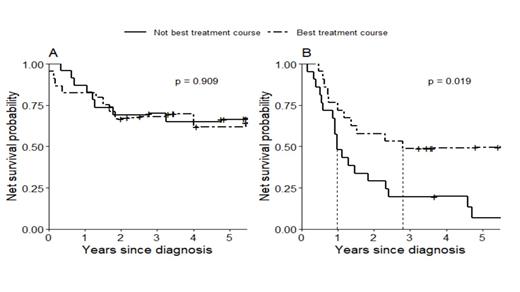
To study the impact of therapeutic decision on overall survival, a case-control study was performed using a one for one matching between group 1 and group 2. An exact matching on individual and disease characteristics (cytogenetic risk, Charlson score class, age group at diagnosis, subtype AML and response to treatment) allowed to pair-match patients following or not the international recommendations for therapeutic strategy. Net survival was estimated until five-year using non-parametric Pohar-Perme estimator (survival distribution compared using Grafféo test).
Results
A total of 1039 AML patients diagnosed from 2012 to 2016 were identified, 449 (43 %) received a curative treatment and 540 patients a non-curative treatment (hypomethylating agents, low dose of cytarabine or other palliative treatment, best supportive care combined to no effective treatment). Based on available clinical data, 430 patients were included in the study.
Group 1 included 296 patients (68%), 167 males and 129 females with 54 receiving allo-HCT (32 geno-identical and 22 unrelated). Group 2 included 134 patients (31%), 72 males and 62 females with 94 receiving allo-HCT (14 geno-identical, 50 unrelated and 30 mismatched).
In patients for whom allo-HCT represented the best option according to the recommendations (Figure B, n = 44), a very significant lower survival was observed in patients who did not receive allo-HCT when they were compared to patients who received allo-HCT, with a 5 year-overall survival probability of 7 % and 50 % respectively (p= 0.019). In patients for whom allo-HCT was not recommended (Figure A, n = 42), we did not observe any significant difference of survival between patients transplanted or not.
Conclusion
This analysis shows the importance of allo-HCT decision in AML patients, especially when following international guidelines. Although individual risks factors have been previously studied, our analysis sums up theses factors and allow to understand the importance of integrating allo-HCT in the therapeutic strategy of AML and to re-evaluate current practices and its impact on patient outcome.
Pigneux: Roche: Consultancy, Research Funding; BMS Celgene: Consultancy, Research Funding; Sunesis: Consultancy, Research Funding; Amgen: Consultancy; Novartis: Consultancy, Research Funding. Forcade: Novartis: Other: travel grant. Mohty: Pfizer: Honoraria; Novartis: Honoraria; Takeda: Honoraria; Jazz: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Gilead: Honoraria; Celgene: Honoraria, Research Funding; Bristol Myers Squibb: Honoraria; Astellas: Honoraria; Amgen: Honoraria; Sanofi: Honoraria, Research Funding; Adaptive Biotechnologies: Honoraria. Dulery: Novartis: Honoraria; Takeda: Consultancy; Gilead: Other: Travel support and registration fees for scientific meetings .

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal