Abstract
Abstract
Introduction:
Thalassemia is one of the most common hemoglobinopathies, with around 5% of world's population expected to have some degree and type of thalassemia. Beta thalassemia (BT) occurs due to a deficient production of the beta-globin chain of hemoglobin. BT is classified into minor, intermedia, and major, defined by their clinical and laboratory findings. Extramedullary hematopoiesis is one of the complications of BT, primarily seen in minor/intermedia subtypes. EMH is the production of blood cells outside the marrow as a compensatory response to longstanding hypoxia. Due to chronic transfusions, it is not expected in patients with beta thalassemia major (BTM). However, there are multiple case reports of EMH in BTM. The incidence of EMH in BTM is thought to be <1%. However, given the increasing cases, it seems that the true incidence is much higher than expected. This systematic review aims to pool the available data and provide cumulative evidence on the occurrence of EMH in BTM patients.
Methods:
This is a systematic review of case reports, series, and retrospective studies that presented data on the occurrence of EMH in BTM patients. Data were recorded and analyzed in Microsoft Excel 2016 and SPSS 26. The protocol has been registered in PROSPERO: CRD42021242943.
Results:
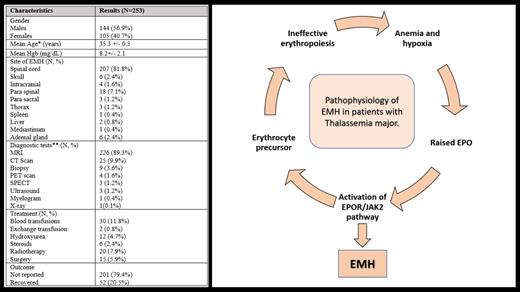
Data from 253 cases of EMH in BTM patients were extracted from 2 retrospective studies and 71 case reports (some of the descriptive data from case reports and most of the descriptive data from retrospective studies was missing). The mean age at presentation was 35.3 +/- 0.5 years. Males constituted 57.7% of the total population. Mean hemoglobin at presentation with EMH was 8.2 +/- 2.1 mg/dL. Lower limb weakness was the most common presenting feature (N=23). Other features included localized pain, urinary incontinence, and an incidental finding of EMH. Magnetic resonance imaging (MRI) was the most widely used diagnostic modality (N=226). However, computed tomography scans, positron emission tomography scans, tissue biopsy, myelograms, and X-rays were also used to diagnose EMH. Various treatments were reported either alone or in combination. Overall, blood transfusion was the commonest reported treatment (N=30), followed by radiotherapy (N=20), surgery (N=15), hydroxyurea (N=12), steroids (N=6), and exchange transfusion (N=2). An outcome was reported in 20% of patients, all recovered, with no reported mortality.
Conclusion:
EMH is considered a rare phenomenon in BTM patients. However, there are many cases reported in which EMH occurred in BTM despite chronic blood transfusions. EMH can occur in any organ system and can present with a varied clinical feature. MRI can effectively diagnose EMH, and conservative management is reported to have similar results compared to invasive treatments. More extensive studies, focusing especially on outcomes, are required to enhance the guidelines on managing EMH in patients with BTM.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal