Abstract
Introduction: The prognosis of classical Hodgkin lymphoma (cHL) is generally inferior in elderly patients (pts) than in younger pts. Tolerance of conventional therapy decreases in elderly pts, and in addition, treatment-related toxicities and death are more common. While the 5-year overall survival (OS) of pts with cHL is 86.6%, this rate is 57.5% in elderly pts.
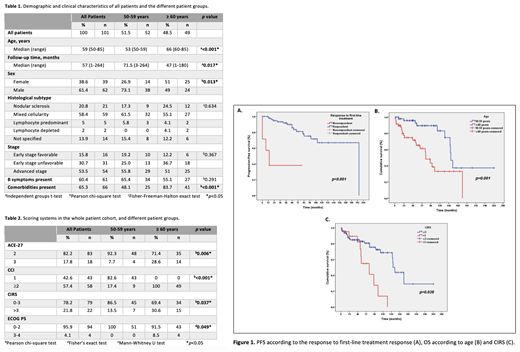
Objective and Methods: The aim of this study was to retrospectively evaluate the demographic, histopathological, clinical, and laboratory features, prognosis determination according to German Hodgkin Study Group (GHSG) in early-stage, International Prognostic Score (IPS)-3 and IPS-7 in advanced-stage, ECOG (Eastern Cooperative Oncology Group) performance scale (PS), Cumulative Disease Rating Score (CIRS) , Charlson Comorbidity Index (CCI), Adult Comorbidity Evaluation-27 (ACE-27) values, treatment responses, toxicities, and survival among cHL pts aged 50 years and older who were diagnosed between 1999 and 2020.
Results: There were 101 pts in total, of which 52 were between 50-59 years of age, and 49 pts were ≥60 years. Sixty-two pts were male, and the most common histopathological subtype was mixed cellularity CHL with 58.4%. Fifty-four pts had advanced-stage disease, while there were 31 and 16 pts with early-stage unfavorable and favorable diseases, respectively. Sixty-one pts (60.4%) had B symptoms (Table 1). ECOG PS, CIRS, CCI, and ACE-27 scores were significantly higher in pts aged ≥60 years than those of 50-59 age group (Table 2). While all pts aged 50-59 years received ABVD as first-line therapy, 79% (n=39) of pts aged ≥60 years had ABVD. Among pts receiving ABVD as a first-line treatment, 82% (n=41) of pts aged 50-59 years and 73.2% (n=30) of pts aged ≥60 years had complete response following first-line treatment (p=0.312). Overall, at interim evaluation, response rates to first-line therapy were significantly higher in pts with IPS-7 value 0-3 (71.8%) than those with IPS-7 value 4-7 (42.9%) (p=0.028). While full-dose treatment was administered to 71 pts (70.3%), 30 pts (29.7%) needed a dose reduction. The percentage of pts needed a dose reduction was 38.8% among pts ≥60 years, whereas this was 21.2% for pts aged 50-59 years (p=0.053). During the follow-up, grades 3-4 hematological and non-hematological toxicities were observed in 50 (49.5%) and 15 pts (14.9%), respectively. Age groups were comparable in terms of hematological and non-hematological toxicities (p=0.369, p=0.127, respectively). None of the pts in the ≥60 age group had received high-dose chemotherapy with autologous hematopoietic stem cell transplantation (HDC with AHSCT)/allogeneic hematopoietic stem cell transplantation (allo-HSCT). On the other hand, 8 pts (15.4%) diagnosed between 50-59 years of age underwent HDC with AHSCT, in one patient (1.9%) allo-HSCT was performed, and one patient (1.9%) received both HDC with AHSCT and allo-HSCT (p=0.004). There was no significant difference in terms of OS between those with and without transplantation (p=0.069). In the multivariate analysis, the risk of progression was higher in pts with lymphocyte ≤600/mm 3 and the risk of mortality was higher in pts with B symptoms (p=0.002, p=0.012, respectively). In addition, progression-free survival (PFS) was inferior in pts who were unresponsive to first-line treatment, and worse OS was associated with higher age and CIRS (p<0.001, p=0.001, p=0.038, respectively) (Fig. 1A-C). During their follow-up, 26 pts (25.7%) died, and the causes of death could be determined in 19 of them. The most common cause of death was treatment complications (n=7). Secondary malignancies were detected in 5 pts, of which 3 died. In 2 pts, the cause of death was HL-related, and 7 pts died due to other causes.
Conclusion: Although not statistically significant, the percentage of pts needing a dose reduction was higher in pts aged ≥60 years, on the other hand, treatment responses and toxicities were similar in both groups, most probably due to personalized treatment selection and dose reduction according to age, comorbidities, and the performance status. Pts undergoing a transplant had a more favorable outcome than pts without a transplant, but the difference did not reach statistical significance. Response to first-line therapy was associated with superior PFS, and pts with higher age and CIRS had inferior OS.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal