Abstract
Background: The development of Richter Transformation (RT) in patients (pts) with chronic lymphocytic leukemia (CLL) while on targeted agents has been reported to have a median survival of 2.3-3.5 months (mo). Treatment is usually anthracycline-based combination regimens, though responses are short-lived. Phase 2 trial of combined venetoclax-REPOCH achieved a median progression free survival (PFS) of 16 mo. We studied the use of ibrutinib in combination with obinutuzumab, cyclophosphamide, doxorubicin, vincristine, and prednisone (I-OCHOP) JUN2017-SEP2018 (ClinicalTrials.gov: NCT03145480). During the conduct of the study, ibrutinib plus RCHOP in untreated diffuse large B cell lymphoma (NCT01855750) reported more treatment-emergent serious adverse events when compared to RCHOP, leading to higher rates of treatment discontinuation with toxicity more prominent in elderly pts. Since the majority of pts with CLL are elderly, enrollment was stopped. We report the outcomes of 3 participants.
Methods: Informed consent was provided through IRB-approved protocol. Subjects were enrolled in an open-label phase II trial combining ibrutinib with O-CHOP. Ibrutinib 560mg was taken daily starting cycle 1 day 1 (C1D1) continuously until progression or start of new anticancer treatment. Obinutuzumab was given per prescription insert starting on C1D1 with CHOP for up to 6 cycles. Pts were allowed to discontinue study drugs to pursue allogeneic stem cell transplant (allo-SCT). Pts aged 18-80 years old with adequate organ function, Eastern Cooperative Oncology Group performance status ≤ 2, and histologically confirmed evidence of RT from CLL were eligible to participate. Prior targeted agent use was allowed until 24 hours prior to dosing. Chemo- or immuno-therapy was not allowed within 21 and 10 days of C1D1 respectively.
The primary endpoint was investigator-assessed overall response rate (ORR) per revised response criteria for malignant lymphoma. Secondary outcomes included hematological improvement, PFS, overall survival (OS), and quality of life. Pts were allowed to pursue allo-SCT after achieving a response and were followed for PFS/OS. Descriptive analyses were utilized, and PFS/OS was calculated from initial treatment to death or last follow-up.
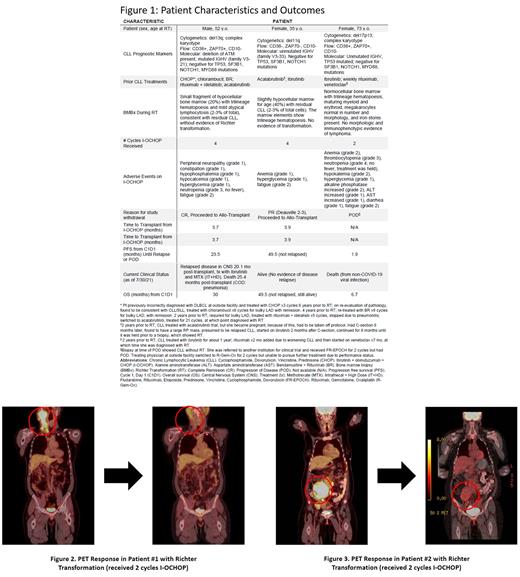
Results: Three pts consented and started therapy: two women and one man with a median [range] age of 53 [36-73] years, all had high-risk disease (Figure 1). Median Cumulative Illness Rating Scale at baseline 2 [0-4]. No large cell lymphoma involved the bone marrow. All pts developed RT while on a novel agent (ibrutinib, acalabrutinib, or venetoclax monotherapy respectively). All enrolled immediately after RT diagnosis and received I-OCHOP. Participants had overall good adherence to ibrutinib therapy (mean missed doses per 28-day treatment cycle was 0.88 doses) while on trial. Two pts developed neutropenia (n=1, grade 3 and n=1, grade 4; neither febrile) that resolved by time of withdrawal from study. 2 pts had anemia (grade 1 and 2), and one participant had thrombocytopenia (grade 2), neither requiring transfusion support. All 3 pts reported fatigue (all grade 2 or less) that on average improved during treatment as assessed by FACIT questionnaire (mean Δ from baseline to end of treatment: -5). Figure 1 lists other adverse events.
Of 3 enrolled pts, 2 pts achieved remission (1 complete, 1 partial) and undetectable minimal residual disease (detection sensitivity 0.01%) in the bone marrow post 4 cycles I-OCHOP and underwent allo-SCT and were followed for progression. Figures 2 and 3 show the PET responses after 2 cycles of I-OCHOP in 2 participants with bulky lymphadenopathy. Time to allo-SCT for the 2 pts was 3.7 and 3.9 mo from C1D1. After transplant, one pt relapsed with RT in the central nervous system after 20 mo and died from pneumonia 5 mo later; the other pt is alive 49.5 mo later with no evidence of disease. The third pt had rapid progression and came off study. Median PFS for the 3 pts was 23.5 mo [1.9-NR] and OS 29.1 mo [6.7-NR] as of datacut July 30, 2021.
Conclusions: Despite historically poor outcomes reported after RT while on a targeted agent, ibrutinib addition to anthracycline-based regimen seemed well tolerated. Two patients achieved a rapid and deep responses irrespective of prior BTK inhibitor use and were able to pursue allo-SCT which correlated with durable PFS/OS.
Rhodes: Conquer Cancer Foundation Young Investigator Award: Other: Grant/Research Support; AbbVie, Genentech, Pharmacyclics, TG Therapeutics: Other: Consultant.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal