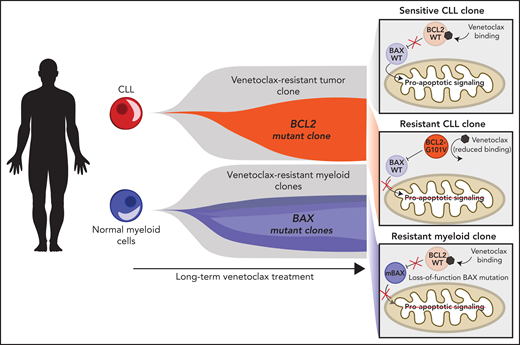
In this issue of Blood, Blombery et al1 identify cytopenias and clonal hematopoiesis in patients with chronic lymphocytic leukemia (CLL) undergoing long-term venetoclax treatment, with unexpected concomitant clonal selection of BAX mutations in normal myeloid cells (see figure).
Schematic representation of clonal expansions in CLL and normal myeloid cells. On long-term venetoclax treatment, CLL cells undergo clonal selection resulting in expansion of the resistant clones harboring mutations in the BCL2 gene, for example, BCL2-G101V. Concomitantly, in the normal myeloid compartment, venetoclax results in clonal selection of BAX loss-of-function mutations (mBAX). Thus, venetoclax results in lineage-specific clonal expansions harboring alternative resistance mechanisms.
Schematic representation of clonal expansions in CLL and normal myeloid cells. On long-term venetoclax treatment, CLL cells undergo clonal selection resulting in expansion of the resistant clones harboring mutations in the BCL2 gene, for example, BCL2-G101V. Concomitantly, in the normal myeloid compartment, venetoclax results in clonal selection of BAX loss-of-function mutations (mBAX). Thus, venetoclax results in lineage-specific clonal expansions harboring alternative resistance mechanisms.
One of the most exciting discoveries in human biology of recent years is that, in fact, we are all genetic mosaics. Vast age-associated clonal mosaicism is observed across healthy tissues,2,3 linked with a wide array of autoimmune, inflammatory, degenerative, and malignant adverse health outcomes.4 Likewise, in the hematopoietic system, somatic mutations previously associated with myeloid malignancies are commonly observed in otherwise healthy individuals.5
Previous work has shown that chemotherapy can select hematopoietic clones harboring PPM1D, TP53, and CHEK2 mutations.6 However, the question of whether strong selection pressure from targeted cancer therapy impact clonal dynamics in healthy tissues remained largely unexplored.
Venetoclax is a potent agent used in blood malignancies, which targets the antiapoptotic protein BCL2. BCL2 inhibition in CLL results in up to a 79% response rate and is effective even in subgroups with adverse prognostic factors, including fludarabine-resistant and TP53-mutated CLL.7 However, long-term treatment with venetoclax can eventually result in expansion of resistant clones, driven by clonal evolution. As is often the case with targeted therapy, mutations arise in the target itself. With venetoclax, mutations in BCL2 that reduce venetoclax binding have been observed in relapsed disease.8 Interestingly, cytopenias may be seen with venetoclax treatment, suggesting that it exerts a selection pressure on the normal hematopoietic system as well.
Blombery et al study a cohort of 92 patients with CLL treated with venetoclax alone or in combination with rituximab. Of note, this cohort was heavily pretreated with fludarabine-alkylator combination chemotherapy. Cytopenias were frequently observed, with a cumulative 5-year incidence of 10.4% of patients progressing to therapy-related myeloid neoplasm (tMN) after venetoclax initiation. As expected, fludarabine-alkylator treatment remained the strongest predictor of tMN progression, as previously described.9 To characterize the clonal dynamics underlying these clinical observations, the authors focused on non-CLL cells and applied error-corrected deep-targeted sequencing of a panel of genes recurrently mutated in clonal hematopoiesis. Mutations were identified in the normal hematopoietic compartment in 83% of the subset of patients with adequate follow-up. Despite an association between clonal hematopoiesis-related mutations and idiopathic cytopenia, the data did not support an association with progression to tMN. In an elegant twist, the authors posited that, given the specific selection pressure of venetoclax, clonal investigation should not be limited to established age-related clonal hematopoiesis drivers. To more closely link hematopoietic clonal dynamics with the therapeutic pressure of venetoclax, they applied targeted sequencing of BCL2 family genes (BCL2, MCL1, BCL2L1, BAK1, and BAX) to samples where the CLL fraction was known to be minimal. Unexpectedly, the authors identified 20 different loss-of-function mutations specifically in BAX across 13 patients. In contrast, BCL2 mutations, which were previously observed in resistant CLL, were not seen in the normal hematopoietic compartment. The observation that recurrent BAX loss of function variants arise in the normal myeloid compartment under the same selection pressure is perhaps the first example of parallel clonal evolution in healthy tissues with targeted cancer therapy. The authors used an in vitro re-expression system to functionally validate that the observed BAX mutations impede venetoclax-induced cell death. Four of 5 variants tested endowed cells with the capacity to resist venetoclax. Therefore, the clonal expansion of BAX mutants in the myeloid compartment can be attributed, at least in part, to increased fitness because of the loss of BAX proapoptotic function.
In their final experiment, the authors perform a longitudinal study of 2 patients who received 7 years of continuous venetoclax treatment. Both patients showed steadily increasing allelic frequencies of BAX mutations over time. The authors then leveraged single-cell sequencing to show that BAX mutations present in a single patient are mutually exclusive at the single cell level, representing 2 independent clonal expansions within the same healthy tissue. This finding is a powerful testimony both to the remarkable genetic diversity that fuels clonal mosaicism and to the strong selection pressure exerted by venetocalx on normal hematopoietic cells. Interestingly, when multiple BAX-mutated clones are observed, the dominant clone was found to be carrying co-occurring clonal hematopoiesis mutations (DNMT3A in one patient and ASXL1 in another patient), suggesting increased fitness. Thus, the strong venetoclax selection pressure in healthy tissue drives BAX convergent clonal evolution, potentially cooperating with canonical clonal hematopoiesis mutations.
Overall, the study by Blombery et al provides robust evidence for the presence of clonal evolution in healthy tissues receiving targeted therapy with venetoclax. This exciting observation raises interesting questions. First, given that the observed BAX mutations are predicted to be loss-of-function, is biallelic loss required for functional impact? The authors infer loss of heterozygosity in high variant allele fraction samples, supporting homozygous BAX loss. Biallelic loss was also the model used in vitro. However, other cases were compatible with heterozygous loss, suggesting that it may be sufficient to impart a fitness advantage. Further studies are needed to definitively link gene dosage with resistance phenotypes. Second, perhaps one of the most exciting observations in this work is the diverging disruption of BCL2 vs BAX in the malignant lymphoid vs the normal myeloid compartments, respectively. What lineage-intrinsic dependencies in the apoptosis pathway drive this observation remains to be determined and may also aid in therapeutic development of apoptosis targeting across blood cancers.
More broadly, this study shows that a strong targeted therapy can select for resistant mutations not only in malignant populations but also in normal tissue clonal mosaicism. As somatic evolution occurs in both normal and malignant cells,2-6,8 the exquisitely focused selection pressure of targeted therapies is likely to impact both. Future studies will reveal if this observation is unique to venetoclax or will be found with other targeted interventions.
Conflict-of-interest disclosure: The authors declare no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal