Abstract
Multiple Myeloma (MM) remains an incurable cancer of terminally-differentiated plasma cells that is universally preceded by the premalignant precursor Monoclonal Gammopathy of Undetermined Significant (MGUS) and later with Smoldering MM (SMM) characterized by greater plasma cell clone volume. The time between the malignant transformation of plasma cell clone to the symptomatic MM, i.e., Latency Period (LP), remains largely unknown for the majority of MM patients. The LP can be affected by age such that MM in younger age patients had a shorter LP than MM diagnosed at an older age. Here, we sought to determine whether the later stage of LP i.e., from SM diagnosis to symptomatic MM. We hypothesize that patients with SM diagnosed at the younger age had faster rate of progression to symptomatic MM.
Methods: The National Cancer Database (NCDB) covers >70% of all cancer patients in the U.S. Since, SMM and MM share the same ICD code, we defined SMM who did not receive any treatment within 3 months following a diagnosis of MM similar to the methods used by others (Ravindran et al. Blood Cancer J. 2016). Initiation of systemic treatment was considered as a surrogate of progression to symptomatic MM. Overall survival (OS) for SM patients was calculated from initiation of systemic treatment after they progressed to MM, estimated by the Kaplan-Meier method, and compared with the log-rank test. Cumulative incidence of progression from SM to MM was calculated with death as a competing risk and compared with the Gray's test. Multivariable Cox and logistic regression analysis were performed to identify independent predictors of OS and progression to MM, respectively.
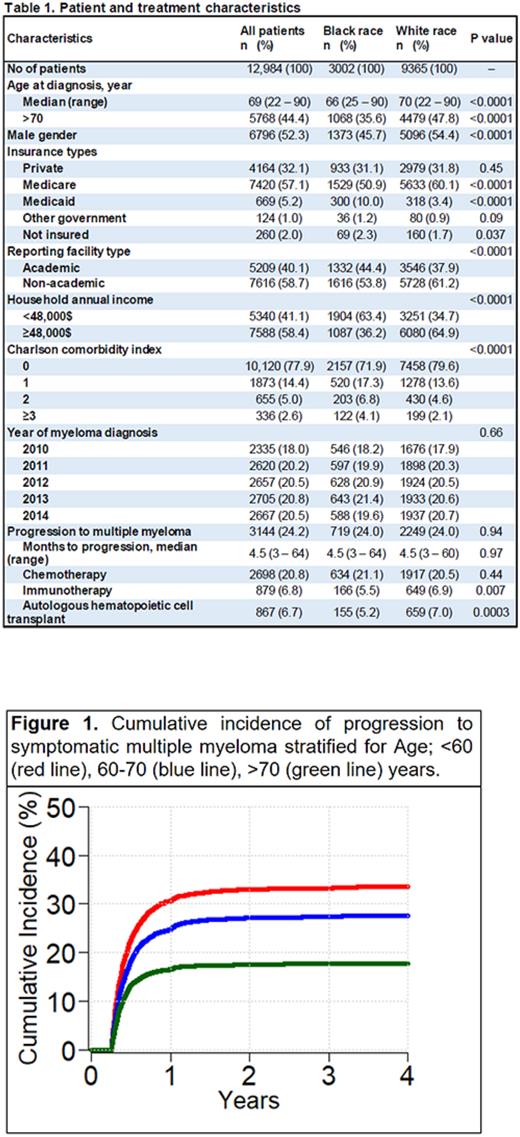
Results: 68,234 patients that had been diagnosed with MM/SMM ICD code were reviewed and, of those, 12,984 patients with SMM were then identified. Among the SMM patients, 3002 (23%) were black, 6796 (52%) were male, and median age at diagnosis was 69 years (range: 22 - 90). SMM patients’ insurance types were private for 4164 (32%), Medicare for 7420 (57%), Medicaid for 669 (5%), and 260 (2%) were uninsured. The majority of the cases were reported from non-academic hospitals (59%). Patient and treatment characteristics are summarized (Table 1). SMM was diagnosed in black patients a median of 4 years younger than in white patients (median age 66 vs 70 years, p<0.0001). Charlson comorbidity index was >2 for 325 (11%) black and 629 (7%) white patients (p<0.0001). Median annual household income of white patients was higher than black patients (p<0.0001). Median time to progression from SMM to MM was 4.5 months (range: 3 - 64). Progression to MM was observed in 3144 (24%) patients during median follow-up of 39 months. All SMM patients received chemo- or immunotherapy after progression and 867 (7%) underwent hematopoietic cell transplant.
The four-year cumulative incidence of progression from SMM to MM patients at ages of <60 vs 60-70 and >70 years was 34% (95% CI: 32 - 35) vs 28% (95% CI: 26 - 29, p<0.0001) and 18% (95% CI: 17 - 19, p<0.0001), respectively (Fig. 1). Four-year cumulative incidence of progression to MM for patients of black and white race was 24.5% (95% CI: 23 - 26) and 24.4% (95% CI: 24 - 25), respectively (p=0.99). Four-year cumulative incidence of progression to MM for patients who were diagnosed between 2010-2012 and 2013-2014 was 25% (95% CI: 24 - 26) and 24% (95% CI: 23 - 25), respectively (p=0.17). On multivariable analysis, each 10-year decrease in age (OR 1.06, 95% CI: 1.05 - 1.06, p<0.0001), white vs black race (OR 1.02, 95% CI: 1.00 - 1.04, p=0.027), and each 1-year decrease in diagnosis year (OR 1.01, 95% CI: 1.00 - 1.01, p=0.015) were associated with progression to MM, however male vs female gender (OR 1.01, 95% CI: 0.99 - 1.02, p=0.26) was not statistically significant.
Conclusions: Taken together, our result indicate the rate of SM to MM progression is independently and inversely associated with age of SMM detection. These findings highlight the potentially longer LP in older patients which can denote more indolent disease in elderly MM patients.
Disclosures
Malek:GSK: Speakers Bureau; janssen: Consultancy; BMS: Speakers Bureau; AdaptiveBio: Consultancy, Honoraria; Amgen: Speakers Bureau; Takeda: Consultancy, Speakers Bureau; Sanofi: Consultancy; Karyopharm: Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal