Abstract
Background Neuropsychiatric effects of Sickle Cell Disease (SCD) are not very well understood. Sickle cells cause vaso-occlusion and ischemic manifestations that can affect various organ systems. The cumulative effect of insults to the brain can be detrimental resulting in potential cognitive delays. Regular blood transfusions and hydroxyurea are established as preventative and therapeutic measures to decrease the risk of cerebrovascular accidents. Strong evidence for timing of screening for brain damage in SCD patients is not available (S C Thust et al). A conditional recommendation from the ASH guideline panel 2020 suggests at least a one-time screening MRI to detect silent cerebral infarcts in adults with SCD (DeBaun MR et al)
Objectives 1. To determine rates of obtaining screening MRI for adult SCD patients enrolled in the Sickle Cell Clinic at Henry Ford Hospital
2. To investigate brain parenchymal changes manifested by Brain MRIs and Head CTs and study associated factors
Methods: We performed a retrospective chart review on 105 patients enrolled in the sickle cell clinic at Henry Ford Hospital who have been followed from June 2013 - June 2022. Baseline characteristics, laboratory findings and presence of comorbidities along with provided therapies are compared among patients with abnormal MRI findings.
Results Out of the 105 patients, 20 (19%) had a Brain MRI done at least once during their lifetime for various reasons. A total of 14/20 MRI reports picked up abnormal findings (70%). Conversely, 44 patients had a CT head done (42%), 17 of which described abnormal findings (39%). Of note, only 4 patients had a transcranial doppler ultrasound, all of which were normal.
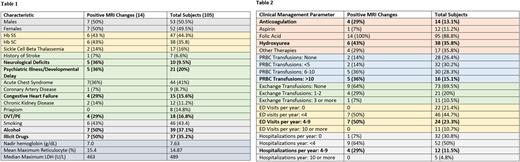
Dissecting those 14 brain MRI reports, 7 cases had ischemic changes/chronic infarcts, 2 cases had white matter changes and 6 cases had other findings including tonsillar ectopia, cerebral and cerebellar volume loss, aneurysms, and degenerative changes. The baseline characteristics as well as clinical parameters of those patients are described in tables 1 and 2.
Looking at the 17 total abnormal head CT reports: 9 cases were described as chronic ischemic changes, 3 hemorrhage cases (one subarachnoid hemorrhage, one subdural and one intracranial hematoma), 2 cases had brain atrophy and 4 cases had other findings including encephalomalacia, punctate hyper-density and trabeculation or lacy appearance of the skull base.
Discussion At least 25% of individuals with SCD will have a neurological complication over their lifetime (Lonergan G et al). Despite paucity of literature looking into prevalence of neuroradiological findings, they have been reported in 44-60% of patients with SCD (Silva et al).
Looking at our center's experience approximately half of the screened patients had chronic ischemic changes reported, which intuitively corelates with silent infarcts known to happen in SCD patients. Patients with neurological deficits and developmental delays are more likely to be screened. Despite the lack of statistical power to extrapolate further, it seemed that patients with abnormal brain MRI reports were more likely to have Congestive Heart Failure and Deep Vein Thrombosis. They also possibly consumed more alcohol and illicit drugs. Those patients were slightly more likely to be on hydroxyurea and had more frequent blood transfusions, emergency department visits and hospitalizations.
Worth mentioning, out of the 14 patients with positive MRI findings, 13 had head CT scans performed concomitantly. 6 of those CT scans reported abnormal findings (46%) and 7 were normal (54%). This infers that there is a high proportion of patients who have normally read head CT scans but have brain parenchymal changes if screened by an MRI.
Conclusions Our center presently screened SCD patients by brain MRI in only 19% of cases. The results of this study help to encourage incorporating and reinforcing the implementation of ASH 2020 guidelines. It is likely that patients with more comorbidities have been screened earlier than others. Detection of neurological complications in SCD may potentially reduce ED visits and hospitalizations if picked up and managed early. Our results propose to re-study patient characteristics on a larger scale once more screening is performed and to compare it with our current data, aiming to have more informative conclusions on SCD patients with neuroradiological findings.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal