Abstract
Background: S-AML patients with prior exposure to hypomethylating agents (p-HMAs) have dismal clinical outcomes and are unfortunately excluded from many clinical trials. Thus, there is no standard-of-care for this high-risk patient population.
Tagraxofusp (TAG; SL-401) is a CD123-directed targeted therapy that carries a truncated diphtheria toxin leading to irreversible inhibition of protein synthesis and apoptosis. TAG is FDA-approved for the treatment of Blastic Plasmacytoid Dendritic Cell Neoplasm. There is high CD123 expression in AML and leukemic stem cells (Jordan, Leukemia 2000); thus, TAG represents a promising investigational therapeutic option. Recent data from the Children's Oncology Group AAML1031 Phase III study revealed that high CD123 expression was associated with high-risk genomic abnormalities and worse clinical outcomes (Lamble, J Clin Oncol 2022). An ongoing study of TAG + azacitidine (AZA) +/- venetoclax demonstrated no dose-limiting toxicities of TAG in newly diagnosed and relapsed/refractory AML/MDS (Lane et al, Blood [Abstract] 2021).
Pre-clinical data suggests that down-regulation of DPH1, a gene responsible for synthesizing diphthamide (the target of the diphtheria toxin), is associated with TAG-resistance. Treatment with AZA hypomethylates CpG motifs in the promoter region of DPH1 which can restore sensitivity to TAG. The combination of TAG and AZA led to prolonged time to progression and overall survival than either agent alone in mouse models (Togami et al, J Clin Invest 2019). However, the optimal administration of TAG and AZA is unknown.
Objectives: The primary objective of this study is to estimate the rate of complete remission (CR) in patients with newly diagnosed S-AML after p-HMAs receiving TAG +/- AZA. Secondary objectives are to describe toxicity, estimate the overall response rate, overall survival, disease free survival, progression free survival, event free survival, and the rate of allogeneic stem cell transplant. Correlative objectives include identifying genomic and single-cell transcriptomic predictors of response, serial assessment of response and MRD with digital PCR, and assessing CD123 expression in responders versus non-responders.
Study Design: Key inclusion criteria are that subjects must be ≥18 years old with newly diagnosed, untreated AML. All subjects must have CD123 expression on leukemia cells by a centralized flow cytometry assay, a documented diagnosis of prior MDS, CMML, MPN, or MDS/MPN overlap syndrome, and have received at least 2 cycles of a HMA. An ECOG performance status of 0-2 and adequate organ function is required (ejection fraction >45%), including an albumin ≥ 3.2 g/dL to mitigate capillary leak syndrome. Key exclusion criteria are subjects who are suitable for and are willing to receive intensive chemotherapy, acute promyelocytic leukemia, and known CNS involvement.
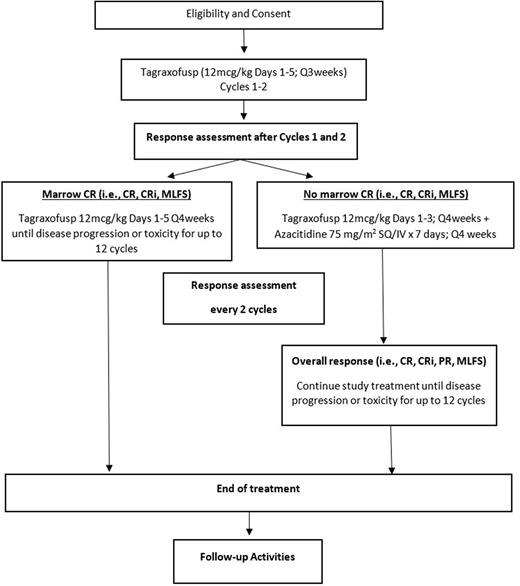
Cycles 1 and 2 will consist of TAG administered at 12 mcg/kg IV daily for 5 consecutive days every 21 days. Subjects who achieve a marrow CR (CR, CRi, CRh, MLFS) after Cycle 2 will continue TAG for up to 1 year at 12 mcg/kg IV for 5 days every 28 days. Subjects without a marrow CR after 2 cycles of treatment will be treated with TAG 12 mcg/kg IV for 3 days + AZA 75 mg/m2 SQ or IV on Days 1-7 every 28 days. Patients without an overall response to TAG + AZA after 4 cycles will be discontinued from study treatment.
Statistical Design: A Simon's two-stage design will be utilized to test the hypothesis that TAG +/- AZA leads to an improved CR rate compared with historical controls. The null hypothesis that the true CR rate is 15% will be tested against one-sided alternative. In the first stage, 23 patients will be accrued. If there are 3 or fewer patients who achieve CR by cycle 6 of therapy, accrual to the study will be stopped to determine the outcome of the study. Otherwise, the study will move on to Stage 2 and 25 additional patients will be accrued for a total of 48 subjects. The null hypothesis will be rejected if 12 or more CR's are observed in 48 patients. This design yields a type 1 error rate of 0.05 and power of 80% when the true CR rate is 30%. Continuous monitoring for toxicity will be performed and the study will be stopped if there is unacceptable toxicity. The trial will begin recruitment as a multi-center investigator-initiated study in the last quarter of 2022 (NCT05442216).
Disclosures
Lai:AbbVie, Agios/Servier, Daiichi-Sankyo, Jazz, Macrogenics, PDS, Pfizer, Genentech, Taiho, Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Astellas, Jazz: Speakers Bureau. Gojo:Ono Pharmaceutical: Membership on an entity's Board of Directors or advisory committees; Clearview: Membership on an entity's Board of Directors or advisory committees; Certara: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees; Immunogen: Membership on an entity's Board of Directors or advisory committees; Celgene: Other: Research support; Genentech: Other: Research support; Gilead: Membership on an entity's Board of Directors or advisory committees, Other: Research support; Amphivena: Other: Research Support; Merck: Other: Research support; Amgen: Membership on an entity's Board of Directors or advisory committees, Other: Research Support; Johnson & Johnson: Membership on an entity's Board of Directors or advisory committees. Foster:Bellicum Pharmaceuticals: Research Funding; Daiichi Sankyo: Consultancy, Membership on an entity's Board of Directors or advisory committees; LOXO Oncology: Research Funding; Macrogenics: Research Funding; Newave Pharmaceuticals: Research Funding; Rafael Pharmaceuticals: Research Funding; Zentalis Pharmaceuticals: Consultancy. Zeidner:AbbVie: Consultancy, Honoraria, Research Funding; Bristol Myers Squibb: Honoraria; Genentech: Honoraria; Gilead: Consultancy, Honoraria, Research Funding; Immunogen: Honoraria; Servier: Consultancy, Honoraria; Shattuck Labs: Honoraria; Arog: Research Funding; Astex: Research Funding; Jazz: Research Funding; Merck: Research Funding; Stemline: Research Funding; Sumitomo Dainippon Pharma: Research Funding; Syndax: Research Funding; Takeda: Research Funding.
OffLabel Disclosure:
Tagraxofusp, approved for the treatment of BPDCN, is being studied here for the purpose of treatment of AML
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal