Abstract
Acute lymphoid leukemia (ALL) is a subtype of acute leukemia which portends a high risk of central nervous system (CNS) infiltration. At the diagnosis, 5-10% of ALL patients have CNS involvement, which has been demonstrated to decrease overall survival (OS). Based on pediatric trials, conventional cytology (CC) has been the standard for CNS disease assessment, although, more recently, flow cytometry (FC) has gained space across several centers. In this study, we intend to: i) access the impact of CNS involvement (defined by CC or FC) on OS, event-free survival (EFS) and relapse of ALL patients treated in a public health center; ii) find variables associated with CNS infiltration in this cohort.
Methods: This retrospective study encompassed 105 cases of ALL newly diagnosed at Instituto do Cancer de Sao Paulo (ICESP). Clinical data were collected from Leukemia clinic database, already approved by Local Ethics Committee. Variables related to cerebrospinal fluid (CSF) were collected from the first lumbar puncture (LP). Traumatic LP was defined as more than 10 red blood cells/µL. CNS status was assessed through the COG's classification and divided into positive/negative for analysis purposes. Patients were treated with different regimens, but intensive intrathecal chemotherapy was given in CNS2 or 3 cases, while cranial irradiation was scheduled for CNS3 patients, only.
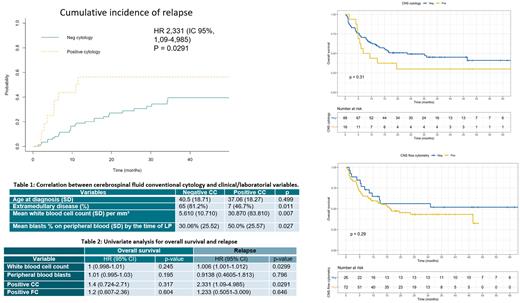
Results: A total of 105 cases were diagnosed from 2014 to 2020. Only one was excluded (death before the first LP). Median age at diagnosis was 37 years (range, 15-79) with a male majority (58%). Most cases had a B-cell phenotype (76%), followed by T (19%) and ambiguous (5%). Philadelphia chromosome was found in 39%. Eighty-nine percent received corticosteroid at the time of LP with a median time of 7 days. Traumatic LP was reported in 50%. CSF resulted positive for disease in 15% (16/104) and 26% (19/72), by CC and FC, respectively. Among those with a positive CC, 56% (9/16) had a traumatic LP. By COG's classification, CNS1, CNS2 and CNS3 were found in 84%, 14% and 2% of cases, respectively. At the time of PL, 44% of patients presented blasts in peripheral blood. By comparing CC and FC, we noticed only one case with CCpos/FCneg whereas 9/19 with FCpos did not have CCpos. Sensitivity and specificity of CC for CNS disease were 53% and 98%. Traumatic LP and positive CC were not statistically correlated (p=0.8) and prior chemotherapy was associated to higher traumatic LP rates (56 vs 31%, p=0.019). Higher white-blood cell (WBC) counts were found in subjects with positive CC or FC (Mann-Whitney test, p=0.007 for CC). Furthermore, the blast percentage was also relevant for CNS positivity (p=0.027). Genetic subgroup, age, CD34 expression and phenotype were not correlated with CNS invasion, among others. Most patients received adapted versions of BFM (n=43), GRAAPH (n=24) and GRAALL-Elderly (n=18) regimens. Five patients received cranial irradiation. Median OS for the whole cohort was 16.4 months, with a 3y OS of 42.5% (95% CI 33.5-54). For BFM subset (Philadelhpia-negative, below 50 years-old), OS and EFS were 53.5% and 37.3%. We did not find correlation between CNS disease with OS or EFS in univariate analysis. Three-year relapse rate was 38.5% (95% CI 29-49) whereas non-relapse mortality (NRM) was 33%. In multivariate analysis, a positive CC increased relapse rate (HR= 2.3 [95% CI 1.1-4.9, p 0.029]). Initial WBC was also correlated with relapse in our cohort. Among relapses, only one was isolated in CNS, while 13 had concomitant bone marrow and CNS involvement. Eighteen patients proceeded to allo-stem cell transplantation so far.
Conclusion: Several studies have demonstrated correlation between CNS infiltration and shorter OS in ALL, even though it relies on how these patients are managed and how CNS is assessed upfront. Our data showed that those who had a positive CSF cytology had a higher risk of relapse, whereas FC was not able to discriminate this risk. Survival rates seem to be increasing over the last years by the adoption of a stratified risk strategy. CSF contamination do not represent a major concern according to our report, as it did not increase CNS involvement or relapse rates.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal