Abstract
Background: Antiphospholipid syndrome (APS) is a systemic autoimmune disease defined by thrombotic or obstetrical events in patients with persistent elevation of antiphospholipid antibodies (aPL) (Lim, 2013). The revised Sapporo/Sydney criteria has been adopted by most professional societies as a guidance to APS diagnosis. To be diagnosed with APS, a patient has to meet at least one clinical criteria and one laboratory criteria. Clinical criteria includes either vascular thrombosis or an adverse outcome during pregnancy. The lab criteria consist of the presence of one or more specified aPL, identified on two or more occasions, at least 12 weeks apart (Miyakis et al., 2006). Antibody testing in patients with suspected APS involves immunoassays for IgG and IgM antibodies to cardiolipin (aCL), and beta2-glycoprotein I (anti-β2GPI), as well as a functional assay for the lupus anticoagulant (LA) phenomenon (Miyakis et al., 2006).
Testing asymptomatic individuals is not recommended and carries a significant rate of false positivity, given that up to 10% of healthy individuals may have transient aPL elevation (Vila et al., 1994). Furthermore, certain medications, infections, malignancies, autoimmune diseases, and rheumatologic diseases can also induce transient elevation of aPL antibodies without associated thrombotic complications, emphasizing the importance of repeated aPL measurements in the diagnosis (Lim, 2013; Rand & Wolgast, 2012). Weakly positive levels of aCL and anti-β2GPI antibodies should not be considered significant. Most authorities require Ab levels to be at or above the 99th percentile to be considered clinically significant (Rand & Wolgast, 2012).
We aim to assess the compliance with revised Sapporo/Sydney criteria in diagnosing APS in our community hospital system.
Methods: We conducted a multi-center, retrospective study among adult patients who were diagnosed with APS in a community healthcare system in southeast Michigan. Demographic and clinical characteristics were collected along with history of venous thrombosis, arterial thrombosis, pregnancy complications, aPL testing results and use of anticoagulants. We used SAS for exploratory data analysis and descriptive statistics.
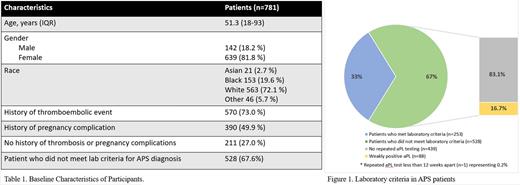
Results: A total of 781 patients were diagnosed with APS between August 2016 to December 2021 (table 1). The median age at diagnosis was 51.3 years (interquartile range 18-93 years). 639 (81.8%) patients were females and 142 (18.2%) were males. Majority of patients were white (n=563, 72.1%). 570 (73.0%) patients had history of venous or arterial thrombosis, 309 (49.9%) had pregnancy complications included in the revised Sapporo/Sydney criteria, and 211 (27.0%) had neither history of thrombosis nor pregnancy complications, not meeting the clinical criteria for APS diagnosis.
528 (67.6%) patients did not meet the laboratory criteria for the diagnosis (figure 1). Of these patients, 439 (83.1%) did not have a repeated testing of aPL antibodies.88 (16.7%) had weakly positive levels of aCL and anti-β2GPI antibodies, below the 99th percentile, and 1 (0.2%) had repeated antibodies testing in less than12 weeks.
Out of 528 patients who did not meet the laboratory criteria, 321 (60.8%) were started on anticoagulants. Of these 321 patients, 135 (42%) did not have any history of thrombosis or other appropriate indication of anticoagulation, such as atrial fibrillation. Of 321 patients who were treated with anticoagulation, warfarin was the most prescribed accounting in 120 patients (37.4%). The remainder of patients (62%) were treated with apixaban, rivaroxaban or enoxaparin.
Conclusion: Our results showed poor compliance with the current guidelines in both selecting the appropriate candidate for testing, and interpreting aPL testing results, leading to an alarmingly high rate of false diagnosis of APS. Obtaining a positive aPL test result in an otherwise disease-free individual can contribute to unnecessary anticoagulation and side effects including bleeding and increased cost burden to patients and families. Therefore, caution must be exercised while ordering aPL tests and adherence to current guidelines should be encouraged in the routine clinical settings.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal