Abstract
Introduction: Burkitt lymphoma is an aggressive non-Hodgkin B-cell lymphoma potentially fatal if left untreated. While the prognosis depends mainly on the histologic features and stage of the disease, it is usually poor in adult patients. The extent to which social determinants of health such as annual median income influence survival outcomes among patients with Burkitt lymphoma needs further exploration. In this study, we described the effect of race/ethnicity and socioeconomic factors on survival outcomes among patients with Burkitt lymphoma in the United States.
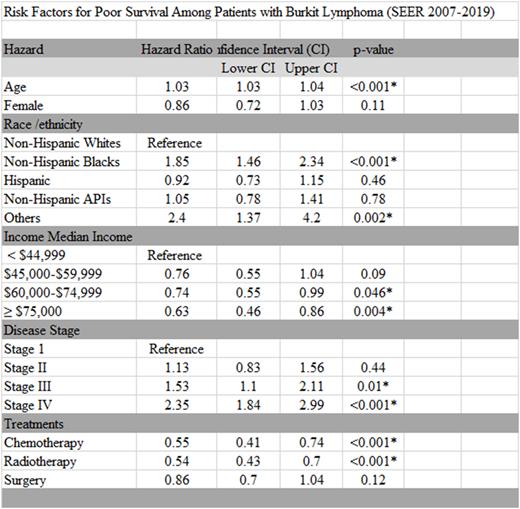
Methods: Using the Surveillance, Epidemiology, and End Results (SEER) 18 Registry, we extracted data on patients with a primary diagnosis of Burkitt lymphoma from 2007 to 2019. The primary outcome of interest was the overall survival of these patients. We utilized the cox regression model to determine the association between patients’ race/ethnicity, age, sex, annual median income, disease stage at presentation and treatment modalities, and overall patient survival. Utilizing the structural equation model, we determined the relative contribution of race/ethnicity, income, and sex to the disparities in survival.
Results: There were 3,578 patients with Burkitt lymphoma with complete survival data in the present study. 60.8% were Non-Hispanic Whites (NHW), 9.6% were Non-Hispanic Blacks (NHB), 19.5% were Hispanics, 8.9% were Non-Hispanic Asian or Pacific Islanders (NHAPI), and 1.4% were of other race/ethnicities. The one- and five-year survival by race/ethnicity was NHW (96.8%, 88.1%), NHB (94.8%,81.8%), Hispanics (97.9%,87.4%), NHAPI (96.7%, 85. 4%). Predictors of worse survival include increasing age, OR= 1.03 (95% CI 1.03-1.04, p <0.001) and racial status as NHB OR=1.85 (95% CI; 1.46-2.34, p= <0.001). Receiving chemotherapy, radiation therapy, and being in the highest income quintiles (defined as an annual income above $60,000) was associated with better survival. In the modeling analysis, the reduced survival among NHBs is partially attributable to lower income and reduced access to treatment modalities. There was no survival disparity by sex; female, OR=0.86 (95% CI 0.72-1.03, p=0.11)
Conclusion: Race/ethnicity, income, and access to chemotherapy and radiation therapy are associated with improved outcomes among patients with Burkitt Lymphoma. Conversely, the association between NHB and reduced survival can be explained by socioeconomic deprivation and lower access to treatment.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal