Abstract
Introduction. The antiphospholipid syndrome is characterized by the presence of anti-phospholipid autoantibodies (aPL) leading to a hypercoagulable state as well as an arterial, venous, and microcirculatory vasculopathy. Under several physiological and pathological situations, including the sickling of red blood cells (RBC), negatively charged phospholipids translocate from the inner to the outer surface of cell membranes leading to the potential generation of the antigenic target of aPL. We tested the following two-part hypothesis: 1) repeated exposure of the immune system of patients with sickle cell disease (SCD) to the antigenic target of aPL leads to an increased formation of aPL; and 2) the presence of aPL is associated with pregnancy and SCD-related complications.
Methods. We conducted a cross-sectional study in 63 adults with SCD who had aPL testing performed during a hospital admission between August 1999 & June 2017. We compared individual aPL levels with categorical and linear variables using the Kruskal-Wallis test and linear regression analysis, respectively. The anticardiolipin (aCL) IgG and lupus anticoagulant (LA) levels were log-transformed for these analyses. An abnormal aPL was defined as any of the following: IgM or IgG anti-b2GPI >20 IU/mL, IgM or IgG aCL > 20 IU/mL, LA > 10 seconds. Clinical complications were compared by abnormal aPL status using the chi-square test.
Results. The median age of the SCD cohort was 32 years (IQR, 21 - 39 years), 49 (78%) were female, 62 (98%) were African American, 5 (8%) had a diagnosis of systemic lupus erythematosus (SLE), 43 (68%) were Hgb SS genotype, 17 (27%) were on hydroxyurea, and 16 (25%) were on chronic anticoagulation therapy. SCD patients with SLE had higher median aCL IgM (6 vs. 1 IU/mL, respectively; P=0.02) and anti-b2GPI IgG (3.5 vs. 0 IU/mL, respectively; P=0.008) levels compared to those without SLE, while lower hemoglobin concentrations were associated with higher aCL IgG levels (β -0.12; P=0.07) and longer LA times (β -0.18; P=0.02).
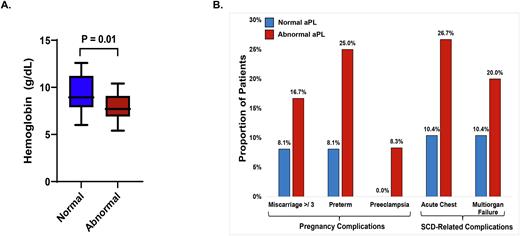
Fifteen of 63 (24%) patients with SCD had an abnormal aPL. Patients with an abnormal aPL had a lower hemoglobin concentration (Figure 1A), a higher white blood cell (WBC; 13.5 vs. 11.8 x109/L, respectively; P=0.06) count, and a lower platelet (268 vs. 340 x109/L, respectively; P=0.05) count at the time of hospitalization compared to those with a normal aPL. A lower hemoglobin concentration (odds ratio [OR], 1.9; P=0.008), a higher WBC count (OR 1.2; P=0.03), and a lower platelet count (10 platelets/µL increment: OR 1.05, P=0.06) were independently associated with the presence of an abnormal aPL by logistic regression analysis, adjusting for age, sex, and prior SLE diagnosis.
Consistent with the second part of our hypothesis, several adverse outcomes trended higher in SCD patients with an abnormal aPL. An abnormal aPL was more prevalent among women with ≥ 3 miscarriages, preterm deliveries, or pre-eclampsia as well as during a hospitalization complicated by acute chest syndrome or multiorgan failure (Figure 1B).
Conclusions. These data support the hypothesis that patients with SCD have a high predilection to form aPL, and that the presence of an abnormal aPL is associated with pregnancy complications and the severity of acute SCD-related complications during hospitalization. Our study is limited by its small number of patients. Further larger studies are needed to assess the mechanisms of aPL generation as well as to determine the prevalence and associated risk of abnormal aPL status in patients with SCD.
Disclosures
Gordeuk:GSK: Consultancy; GBT: Consultancy, Research Funding; Forma: Consultancy; CSL Behring: Consultancy, Research Funding. Saraf:Global Blood Therapeutics: Consultancy, Research Funding, Speakers Bureau; Agios: Consultancy; ORIC: Consultancy; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; FORMA Therapeutics: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal