Abstract
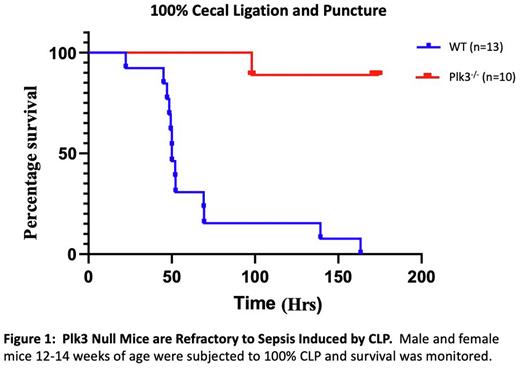
Sepsis is the most expensive condition in US hospitals and carries a mortality rate of 26%. Sepsis, which is the body's response to overwhelming infection, can lead to septic shock, which is characterized by thrombocytopenia, hypotension, and organ damage. The progression of sepsis is multifaceted, involves many cell types including platelets, and is not well understood. Polo-like kinases (Plk) are evolutionarily conserved serine/threonine kinases that are multifunctional, though their most well characterized function is cell cycle regulation. Plk3 is expressed in platelets and megakaryocytes, but its role in immune function is unknown. We used Plk3-/- and WT animals to evaluate the function of Plk3 as it relates to sepsis. Using a model of systemic inflammation (18 mg/kg LPS), we found that Plk3-/- mice are completely refractory to LPS and experience zero mortality, while WT mice succumb within 24 hours. To determine whether this resistance extends to polymicrobial infection, we performed cecal ligation and puncture (CLP) on WT and Plk3-/- mice. We found that 50% of WT mice die within 48 hours of surgery and that 100% of WT mice eventually succumb, while Plk3-/- mice have only 7% mortality over the course of the experiment (Figure 1). Furthermore, 48 hours after surgery WT mouse shock scores indicate that all mice were in septic shock, while Plk3-/- mice had shock scores equal to that of sham operated mice. Interestingly, an analysis of peritoneal bacterial load revealed that 24 hours after CLP, WT mice had 2.5-7 X 105 CFU/mL, while bacterial colonies were virtually undetectable in the peritoneum of Plk3-/- mice. Similar results were observed in the blood of WT and Plk3-/- mice. To determine if alterations in gut microbiota contribute to reduced bacteremia observed in Plk3-/- mice following CLP, we performed cecal slurry injections whereby cecal contents from WT mice were injected IP into Plk3-/- mice and vice versa. In each case our data mirrored that of CLP as WT mice succumbed within 48 hours, while Plk3-/- mice survived indefinitely. It is known that platelet reactivity is heightened during the initial phases of sepsis, which contributes to micro thrombus formation and eventually thrombocytopenia. Therefore, we analyzed platelet deposition in the lung 24 hours after CLP in WT and Plk3-/- mice. We found significantly less platelet deposition in lungs from Plk3-/- mice compared to lungs from WT mice. In fact, platelet deposition in Plk3-/- mouse lungs was not different from that of sham operated mouse lungs. These data suggest that platelet reactivity is unaltered in Plk3-/- mice as a result of sepsis. It will be interesting to determine if that is the primary cause of Plk3-/- mouse survival following CLP. Collectively, our data suggest that Plk3 is a primary regulator of the body's response to bacterial infection.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal