Abstract
The metabolic state of leukemic cells can be defined by driver mutations and determine susceptibility to therapy. Metabolic rewiring is an essential feature of cancer cells to promote survival in adverse conditions and can be exploited as a therapeutic vulnerability. We previously showed metabolic adaptation upon PDK1 or complex II inhibition in FLT3-ITD Acute Myeloid Leukemias (AML) (Erdem et al, 2022). Mutations in Isocitrate Dehydrogenase (IDH1/2), an enzyme responsible for converting isocitrate into α-ketoglutarate (αKG), are found in about 20% of AML cases. These mutations can also impact on cellular metabolism due to their role in the tricarboxylic acid (TCA) cycle and abnormal production of 2-R-hydroxyglutarate, a competitive inhibitor of αKG-dependent enzymes, resulting in chromatin hypermethylation. However, the metabolic consequences of IDH mutations are still largely unknown. Here, we investigated the metabolic state of IDH1/2 mutant cells with the ultimate aim to uncover targetable vulnerabilities.
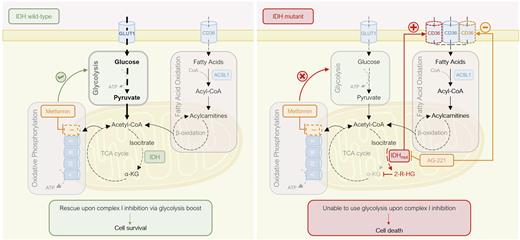
To explore potential metabolic targets associated with IDH2 mutations, we performed RNA sequencing in CRISPR/Cas9 gene-edited isogenic TF1wt and IDH2R140Q cells. The top differently expressed genes were associated with fatty acid (FA) oxidation (FAO), such as CD36, a major FA transporter, and ACSL1, responsible for converting FAs into fatty-acyl-CoAs. Gene Set Enrichment Analysis associated the transcriptome of IDH2R140Q cells with processes related to increased mitochondrial complex I activity and FA biosynthesis. To functionally validate our findings, we performed a drug screen targeting the main metabolic pathways. Metformin, an FDA-approved drug known to inhibit complex I, selectively induced apoptosis in IDH2R140Q cells. Treatment with triacsin C, an ACSL1 inhibitor, reduced cell proliferation in the mutant cells, whereas 2-deoxyglucose, a glycolysis inhibitor, had no significant effect in this population. In contrast, TF1wt largely depended on glycolysis, indicating a metabolic rewiring after IDH2 mutation. Moreover, we confirmed by flow cytometry higher surface expression of CD36 in IDH2R140Q cells, which was downregulated upon treatment with FAO inhibitors and AG-221, an IDH2 inhibitor. Altogether, our data suggest that IDH2-mutant cells heavily rely on mitochondrial respiration, whereby FAs act as the main carbon source for this pathway.
We then assessed oxygen consumption (OCR) and extracellular acidification (ECAR) rates by Seahorse analysis. In steady state, mitochondrial respiration was similar between TF1wt and IDH2R140Q cells, and blocking complex I with metformin significantly reduced OCR in both cell lines. However, its effect on cell viability was much more pronounced in IDH2R140Q cells. Interestingly, WT cellsshowed increased basal ECAR after treatment, suggestive of a shift towards glycolysis, unobserved in the mutant cells. We measured glucose consumption and lactate production in the cellular media, which confirmed a higher glucose uptake and lactate secretion only in the WT setting. Gene expression analysis revealed up-regulation of the glycolysis-related genes ALDO and PFKFB3 in WT but not IDH2R140Q cells upon treatment. Altogether, these data further confirm a metabolic rewiring of IDH2R140Q cells that now depend less on glycolysis to drive mitochondrial respiration.
Next, we confirmed our findings in primary AML samples harboring IDH1/2-mutations. Treatment with metformin followed by Seahorse showed similar results as observed in theTF1 models. We previously developed a technology based on differential membrane protein expression that allowed us to identify and prospectively isolate NPM1cyt/IDH1R132H from NPM1cyt/IDH1wt subclones within an individual patient for functional studies (de Boer et al, 2018). RNA-seq analysis revealed distinct transcriptional signatures whereby the IDH1R132H clone was associated with processes related to mitochondrial and FA metabolism, and displayed a 3-fold higher expression of CD36 in comparison to the IDH1wt clone.
While most mutations in cancer often lead to metabolic flexibility, our findings suggest that IDH1/2-mutant AMLs induce metabolic rewiring, but are less prone to readapt under stress conditions. Consequently, we uncover the lack of metabolic plasticity as the mechanism behind the usage of complex I inhibition as therapeutic vulnerability in IDH1/2-mutant AMLs.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal