Abstract
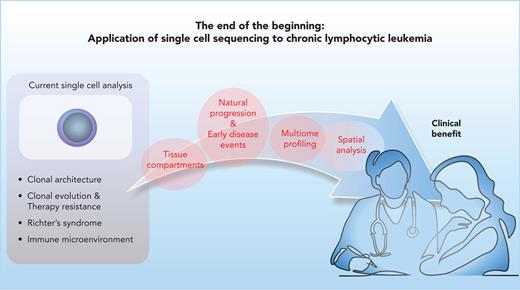
Single-cell analysis has emerged over the past decade as a transformative technology informative for the systematic analysis of complex cell populations such as in cancers and the tumor immune microenvironment. The methodologic and analytical advancements in this realm have evolved rapidly, scaling from but a few cells at its outset to the current capabilities of processing and analyzing hundreds of thousands of individual cells at a time. The types of profiling attainable at individual cell resolution now range from genetic and transcriptomic characterization and extend to epigenomic and spatial analysis. Additionally, the increasing ability to achieve multiomic integration of these data layers now yields ever richer insights into diverse molecular disease subtypes and the patterns of cellular circuitry on a per-cancer basis. Over the years, chronic lymphocytic leukemia (CLL) consistently has been at the forefront of genomic investigation, given the ready accessibility of pure leukemia cells and immune cells from circulating blood of patients with this disease. Herein, we review the recent forays into the application of single-cell analysis to CLL, which are already revealing a new understanding of the natural progression of CLL, the impact of novel therapies, and the interactions with coevolving nonmalignant immune cell populations. As we emerge from the end of the beginning of this technologic revolution, CLL stands poised to reap the benefits of single-cell analysis from the standpoints of uncovering fresh fundamental biological knowledge and of providing a path to devising regimens of personalized diagnosis, treatment, and monitoring.
Introduction
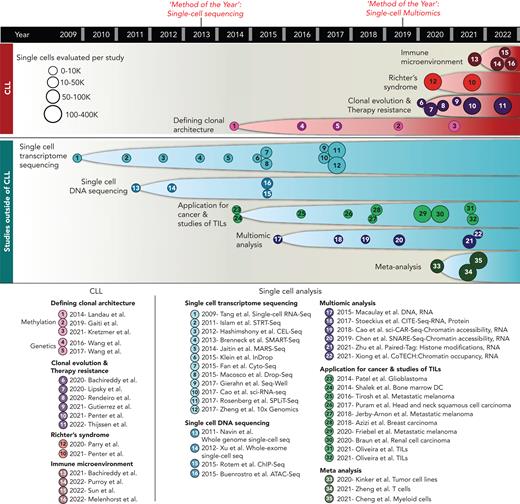
In 2013, single-cell sequencing was selected as Method of the Year by Nature Methods,1 on the heels of growing technical innovations that would enable the broad accessibility of robust protocols for the sequencing of DNA2-5 and RNA6-17 of single cells (Figure 1). It was recognized that the widespread adoption of such approaches would transform vastly our understanding of cellular identity and heterogeneity and would impact our understanding of the plasticity and regulation of both normal and diseased cells. In the ensuing years, we have witnessed the dramatically rapid pace at which this technology has evolved. In less than a decade, the implementation of innovative approaches and commercial support have enabled the broad dissemination of high-throughput sequencing capabilities, such that it is now feasible to profile hundreds of thousands of individual cells and thereby gain a comprehensive bird’s-eye view of the composition of diverse tissue types.4,5,10-17 Moreover, the diversity of single-cell profiling approaches has proliferated, ranging from methods to evaluate a single data layer to growing approaches to measure simultaneously the genome, transcriptome, epigenome, and proteome at single-cell resolution18-23; indeed, single-cell multiomics was lauded as the Method of the Year in 2019.24
Timeline of single-cell sequencing technology development and its applications to CLL research. (top) Major discoveries in CLL through single-cell sequencing. (bottom) Milestones in single-cell sequencing and as applied to cancer biology and tumor immunology. TIL, tumor-infiltrating lymphocytes.
Timeline of single-cell sequencing technology development and its applications to CLL research. (top) Major discoveries in CLL through single-cell sequencing. (bottom) Milestones in single-cell sequencing and as applied to cancer biology and tumor immunology. TIL, tumor-infiltrating lymphocytes.
It has been well-recognized that single-cell approaches are most richly able to provide insight in settings of cellular complexity and heterogeneity, such as cancer and analysis of tissue immune microenvironments, where analysis of bulk populations otherwise would obscure the distinct biological contributions of rarer cellular subpopulations. Altogether, the field of cancer research (and other fields of biology as well) has benefited from this transformative technology, such that we have accelerated our understanding of intratumoral cellular heterogeneity, therapeutic resistance, and mechanisms of tumor and immune cell cross talk of individual cancers25-31 as well as across multiple cancers,32,33 and the analysis of tumor-infiltrating lymphocytes.34,35 For chronic lymphocytic leukemia (CLL), which is marked by clonal expansions of mature B lymphocytes in the blood, marrow, and lymph nodes, the concept of single-cell analysis has been a long-valued component of clinical care. Indeed, the characterization and quantitation of individual cells by approaches such as karyotyping,36 fluorescence in situ hybridization,37 and flow cytometry long have been in place as clinical assays used for diagnosis and prognostication for this malignancy.38,39
Over the past decade, much progress in the molecular understanding of CLL has been gained through large-scale bulk analyses of CLL through profiling by next-generation sequencing. Altogether, these studies of increasingly larger sample numbers (most recently up to >1000 patients)40 have enabled the unraveling of the genetic41-47 and epigenetic48-50 heterogeneity of CLL and the integrative analysis of genetic, transcriptional, and epigenetic information. Altogether, these studies have defined the distinct molecular features of CLL disease subtypes and their relationship to clinical outcomes. More recently, the architecture and evolutionary trajectories of Richter’s syndrome (RS), arising in the subset of patients with CLL who have undergone high-grade transformation to diffuse large B-cell lymphoma (and less commonly Hodgkin lymphoma), also have been profiled increasingly by bulk sequencing methods, leading to improved understanding of the genetic pathways underlying this biological process.51-53
CLL is now poised to take advantage of the considerable foundation of innovation that has been established from single-cell analysis technologies. As reviewed herein, studies have already started to harness single-cell technology to investigate the CLL-intrinsic properties driving disease initiation and progression,54,55 with analysis of the clonally evolved cell populations at baseline and after therapy.56,57 Furthermore, new studies also have been undertaken to gain understanding of the CLL immune microenvironment58,59 and its role in response and resistance to therapy.60,61 We assert that with the many maturing developments in single-cell technologies, we are now at the end of the beginning of single-cell research for CLL. That stated, much more remains to be explored, especially as platforms for increasingly multidimensional analysis of individual cells continue to develop. We review key developments and innovations and the challenges confronted by the CLL research community in the current single-cell genomics era. We highlight how these new approaches are impacting our understanding of the pathophysiologic features and clinical behavior of CLL and how they may serve to guide the selection of optimal therapeutics and help to improve patient outcomes.
Single-cell technologies to dissect native CLL heterogeneity
The protracted clinical course and varied natural history of CLL and the ready accessibility of pure populations of CLL cells simply by venipuncture (Figure 2A) have enabled the consistent presence of CLL at the forefront of large-scale genomic characterization. Studies of whole-exome sequencing of hundreds of CLL samples previously identified a broad spectrum of recurrently mutated genes (eg, TP53, ATM, SF3B1, IKZF3, NOTCH1, MYD88, and others), including recurrent mutations in noncoding regions,41,43-47 as well as delineated the presence of extensive genetic and epigenetic heterogeneity45-47,49,62 that forms the basis of clonal evolution in this disease. The definition of clonal and subclonal events in CLL using bulk sequencing platforms has relied on innovations in computational inference to identify cell subpopulations, to calculate their distinct kinetics that contribute to varied disease trajectories,63 and to infer the link between molecular features and phenotypic properties.
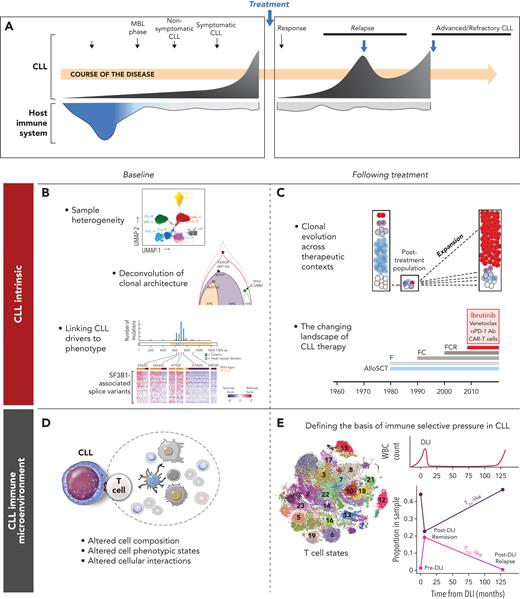
Insights into CLL afforded by single-cell analysis. (A) Schematic of a typical CLL disease course and conceptualization of the coevolution with host immunity. Thus far, single-cell analysis has been applied to evaluate the molecular features intrinsic to CLL cells at baseline (B) as well as after therapy (C). Likewise, single-cell analysis has been applied to evaluate the native state of the CLL immune microenvironment (D) as well as the dynamic changes in immune cell populations after immune therapies (E). WBC, white blood cell.
Insights into CLL afforded by single-cell analysis. (A) Schematic of a typical CLL disease course and conceptualization of the coevolution with host immunity. Thus far, single-cell analysis has been applied to evaluate the molecular features intrinsic to CLL cells at baseline (B) as well as after therapy (C). Likewise, single-cell analysis has been applied to evaluate the native state of the CLL immune microenvironment (D) as well as the dynamic changes in immune cell populations after immune therapies (E). WBC, white blood cell.
With single-cell characterization, the core property of clonal heterogeneity at both DNA and RNA levels has been delineated more reliably with far greater resolution than ever before. Characterizations of single cells from collections of individual CLL samples have revealed interpatient transcriptome and methylome heterogeneity.54,64-66 Single cells derived from the same patient consistently have been found to cluster quite distinctly from those of other patients,66,67 and these distinct phenotypes per each CLL seem to be stable across time because they are maintained in the transition from early preleukemic B-cell expansions (monoclonal B-cell lymphocytosis [MBL]) to CLL (Figure 2B).66 By contrast, nonmalignant immune cells across patients have been found to be transcriptionally similar.56,66 Interpatient CLL heterogeneity likewise has been demonstrated at the level of the methylome66 and chromatin accessibility56 through the detection of mitochondrial DNA (mtDNA) mutations using the assay for transposase-accessible chromatin sequencing.68
The coexistence of clonal and subclonal CLL populations implies a temporal ordering of genomic events over its natural history. Somatic single nucleotide variants provide natural molecular “barcodes” to define the clonal relationships among cancer cells. Some of the earliest studies used to establish cancer phylogeny in CLL used targeted single-cell reverse transcription polymerase chain reaction analysis to detect robustly the presence of somatic mutations among hundreds of CLL cells. These studies largely have validated methods of computational inference for phylogeny54 and also have demonstrated the phenotypic consequence of somatic mutations. For example, this technique demonstrated that the same individual cells expressing mutation in the key spliceosome component SF3B1 were the same ones definitively expressing those altered splice transcripts previously associated with this mutated driver.54,55 Higher throughput approaches to link genotyping with single-cell transcriptomes have been developed since, such as genotyping of transcriptomes69 and others.70,71 Moreover, the use of epigenomic data to construct CLL lineage trees based on stochastic DNA methylation changes65 and naturally occurring mtDNA mutations have been demonstrated to mark and track subclone populations. Potential limitations using this technique may arise from horizontal transfer of mitochondria between cells, although the extent of this process seems to be rather limited.72 In a study applying this approach to bone marrow-derived mononuclear cells, mtDNA mutations detected in CLL cells also could be tracked back to early progenitor cells possessing capacity for multilineage differentiation.73 These studies support the notion that although CLL is recognized as a malignancy of mature B cells, its cell of origin may be far earlier in the hematopoietic lineage tree, as suggested in previous reports.74,75 Likewise, mtDNA mutations have been demonstrated to enable the tracing of transformation of a CLL subclone into RS.56 Single-cell analyses enable the characterization of intratumor heterogeneity at greater resolution. However, the current challenge is the linking of this high-resolution information to cell fate and clonal origin to gain understanding of therapeutic response. This has led to the development of lineage tracing approaches,57,76,77 providing the opportunity to deepen our understanding regarding clonal evolution in CLL.
Defining the impact of therapy on CLL cells
The last few years have witnessed a major sea change in the therapeutic offerings available to patients with CLL. Whereas chemotherapy-based regimens such as fludarabine, cyclophosphamide, and rituximab until recently were considered standard-of-care first-line therapies,78 the introduction of targeted inhibitors of the B-cell receptor (BCR) and B-cell lymphoma 2 signaling pathways (eg, ibrutinib and venetoclax, respectively)79,80 has changed the treatment landscape of CLL dramatically in the last few years. Notwithstanding the availability of these targeted agents, allogeneic hematopoietic stem cell transplantation (HSCT) has remained an important therapeutic method for younger and fitter patients with multiple relapsed or refractory or poor-risk CLL (Figure 2C).81-83
In surveying the impact of these various therapies, in which the trajectories of individual CLL subclones were tracked over time using mtDNA mutations and chromatin accessibility signatures, the extent of clonal evolution was most striking in the setting of intensive therapeutic bottlenecks, such as during chemoimmunotherapy or after allogeneic HSCT, compared with continuous therapies such as targeted inhibitors (eg, ibrutinib).56 The changes in mtDNA mutations after chemotherapy were paralleled by the acquisition of additional copy number variants and chromatin alterations and were associated with profound shifts in transcriptional state. In a separate study of clonal diversification and adaptation to CLL chemotherapy, a novel system for functionalized lineage tracing that integrates DNA barcoding with single-cell RNA sequencing and clonal isolation (ClonMapper) was introduced into chemotherapy-treated CLL cell lines.57 Single-cell analysis of samples collected at serial time points revealed the distinct trajectories of extinction and expansion of particular subclones in relationship to treatment exposure, as well as the overall profound genomic diversification of the CLL population after chemotherapeutic treatment. High survivorship subpopulations exhibited unique transcriptomic signatures associated with the upregulation of CXCR4, Wnt, and Notch signaling.57 Single-cell‒based deconvolution of high- vs low-survivorship subpopulations further revealed distinct clonal dynamics and evidence of interactions among distinct CLL subclones, impacting the overall CLL growth dynamics.
A number of studies have evaluated the impact of targeted inhibitors on CLL response and resistance. One study integrated single-cell and long-read RNA sequencing and revealed myeloid leukemia cell differentiation protein as a direct transcription target of NF-κB and that myeloid leukemia cell differentiation protein upregulation led to venetoclax resistance in a relapse cohort of patients with CLL.71 A separate study combined single-cell immunophenotypic, transcriptomic, and chromatin mapping of the molecular and cellular dynamics of CLL and immune cells on ibrutinib treatment using longitudinal peripheral blood samples. The analysis of the CLL cells revealed reduced NF-κB binding signatures as well as reduction of lineage-defining transcription factors (EBF1, FOXM1, IRF4, PAX5, and PU.1) on ibrutinib exposure. Ibrutinib treatment led both the CLL and peripheral blood T cells to exhibit a shared, quiescence-like gene signature (containing CXCR4 and ZFP36L2), whereas monocytes and macrophages displayed upregulation of inflammatory genes associated with chromatin accessibility changes.67 Regarding resistance mechanisms, the use of targeted mutation detection revealed early clonal shifts associated with disease progression after ibrutinib treatment, with detection of subclonal mutations in BTK, PLCG2, and ITPKB at the time of relapse.84 More extensive analyses have revealed disease progression after venetoclax and Bruton tyrosine kinase inhibitors frequently to be oligoclonal, characterized by multiple coexisting subclones each harboring a distinct resistance mutation.85
The therapeutic basis of allogeneic HSCT relies on the recognition and eradication by donor-derived immune cells of recipient leukemic cells (graft versus leukemia [GvL] effect), but relapse remains a major source of treatment failure.86,87 A recent single-cell transcriptome-based analysis of CLL dynamics during the course of allogeneic HSCT relapse revealed the genetic and epigenetic trajectories underlying the distinct kinetics of disease relapse.60 Although early relapsed CLL (within months of HSCT) was genetically and transcriptionally stable and was characterized by a pre-existing stem-like transcriptional state driving the resistance to GvL, late relapse (approximately 2 years from HSCT, and hence defined as acquired resistance to GvL) displayed neoantigen depletion and diverging genetics and an epigenetic state compared with pretreatment disease. Of note, the extent of methylome remodeling was far greater after such exposure to immunologic selective pressure compared with a comparator cohort relapsing after combination chemotherapy. Thus, the mechanisms of clonal escape in CLL can be distinguished based on exposure to distinct treatment methods.
Interrogating the role of the immune microenvironment on natural CLL progression
Increasing lines of evidence have highlighted the role of the immune microenvironment on the behavior of tumor cells and of the molecular interplay between tumor and immune cells.88-90 CLL long has been considered a prototypic tumor with high dependence and extensive cross talk with diverse immune cell subtypes in its tumor microenvironment (TME; previously reviewed extensively).91 In particular, nurse-like cells, which are tumor-associated macrophages that exhibit an M2-like phenotype, promote CLL survival through secretion of CLL-supportive chemokines and ligands such as B-cell activating factor and a proliferation-inducing ligand.92,93 Follicular dendritic cells present unprocessed antigen to B cells via complement receptors 1 and 2, activating BCR signaling and promoting CLL survival. In the past, CLL cells often are thought to exhibit low immunogenicity because of acquired T-cell dysfunction that progresses throughout the disease course. However, in recent years, T-cell‒mediated anti-CLL immune responses have been demonstrated in various settings, both within the Eμ-TCL1 model94 and in the context of response to ibrutinib,95 allogeneic HSCT,96 and whole CLL cell vaccination,97 and possibly among the rare cases of spontaneous CLL regression, emphasizing the multidimensional role of T cells in the CLL TME.98,99
Most past studies to dissect the CLL TME have focused on the characterization of only a few of the many immune cell subtypes present in patients, whereas single-cell analysis is well equipped to provide a bird’s-eye systems-level assessment of the disease state (Figure 2D). A recent study of single-cell transcriptomes compared circulating non-CLL immune cells from healthy donors (HDs), individuals with MBL, and patients with CLL at baseline. The proportion of CD8+ effector memory T cells was found to be higher in patients with CLL than in HDs, with a corresponding decrease in CD4+ central memory T cells. Additionally, interactome analysis revealed an increased number of immune inhibitory signals between CLL and the increased myeloid population in peripheral blood mononuclear cells of patients with CLL. Moreover, these changes already were present in preleukemic MBL samples, emphasizing that such immune disruptions already are manifest early in the natural history of CLL.59
A functionally active compartment harboring CLL cells is the lymph node, a specialized microenvironment in which BCR and NF-ĸB signaling are active in driving CLL proliferation.100 Conversely, CLL cells are known to modulate their surroundings by secreting chemokines to attract tumor-supporting immune cells, which in turn promote tumor survival.101 Such tumor-immune cross talk within the CLL lymph node microenvironment recently was investigated at the single-cell level. An expression signature of cellular proliferation in CLL cells was associated with the presence of M2 macrophages and CD4+ memory T-cell populations, suggesting their role in sustaining aggressive CLL disease.102 A potential limitation of this study is the high proportion of CLL cells within these lymph node samples (median, 77.9%). Given the importance of lymph node biological features in CLL and yet the limited number of studies of the CLL lymph node microenvironment, phenotypic characterization of this population is a rich area for future investigation.
Defining the shifts in the CLL immune microenvironment after therapy
The mechanisms underlying therapeutic resistance mediated by the immune microenvironment are becoming clearer with the use of single-cell analysis, providing insights into the effects of selective therapeutic pressure and identifying candidate biomarkers of response.
One study applied single-cell transcriptome profiling to define the mechanisms of resistance to ibrutinib and identified LGALS1 (galectin 1) and LAG3 (lymphocyte-activating gene 3) as candidate genes associated with resistance. Ibrutinib-sensitive cells displayed less interactions with monocytes, natural killer, T, and dendritic cells compared with ibrutinib-resistant cells, suggesting that the resistant CLL cells collaborate with other immune cell populations to form a CLL-protective niche.103 Consistent with this finding, a separate study identified a decrement in the number of immune inhibitory signals (eg, CTLA4, LGALS9, and TIM3) between CLL and various immune cell subtypes after ibrutinib exposure, supporting the notion that ibrutinib sensitivity is mediated by immune microenvironmental cross talk.59 After ibrutinib treatment, T cells of patients with CLL have been found to exhibit a quiescence-like gene signature, whereas monocytes and macrophages display upregulation of inflammatory genes, both associated with distinct changes in chromatin accessibility and thought to be mediated by the off-target inhibition of kinases other than BTK.67
Defining the changes in reconstituting immune cell populations such as T cells after allogeneic HSCT for CLL has the potential to reveal mechanisms underpinning immune-mediated antitumor control. In a study in which mtDNA mutations were used as natural barcodes in longitudinal samples collected from patients with CLL, including those treated with allogeneic HSCT, these molecular markers were found to mark expanded donor-derived CD8+ effector memory T cells.56 Such characterizations demonstrate the potential of single-cell mtDNA mutation detection to track donor and recipient interactions among diverse reconstituting immune cell populations and highlight immune microenvironment function during the course of CLL therapy.56 In a separate study focused on the large-scale analysis of marrow-infiltrating immune cell populations before and after donor lymphocyte infusion, an established adoptive cellular therapy for treatment of relapsed disease after HSCT, the clonal dynamics of diverse T-cell populations from patients with relapsed chronic myelogenous leukemia and CLL were evaluated.58 Donor lymphocyte infusion (DLI) responders were found to have higher proportions of terminally exhausted T cells at baseline compared with DLI nonresponders. This cell population has been described as possessing relatively greater cytotoxicity but a shorter life span compared with precursor exhausted T cells, which were found to be expanded after DLI in responders (Figure 2E).
Analysis of exceptional responders to immunotherapy, for instance patients with CLL showing a durable response to CD19-targeting chimeric antigen receptor (CAR) T-cell infusions, has the potential to provide insight into the determinants of effective anti-CLL immunity.104,105 For instance, a recent longitudinal analysis of peripheral blood mononuclear cells by single-cell sequencing from 2 exceptional responders across more than 10 years after initial CAR T-cell infusion revealed 2 distinct phases of anti-CLL immune response: an initial response phase mediated by CD8+ or γδ CAR-T cells, followed by a subsequent phase mediated by a highly activated CD4+ CAR T-cell population exhibiting cytotoxic characteristics such as the upregulation of perforin 1, granzyme K, and granzyme A, along with increased functional proliferation, metabolic activity, and cytokine expression. In vitro response to CD19 expressing cells suggested that these long-persisting CD4+ CAR T cells remained functionally active, providing a long-term antileukemic response. CAR T-cell characterization in this study thus reveals important immune cellular properties associated with long-term CLL control.106
Despite advances in CLL treatment, the transformation of CLL to aggressive B-cell lymphoma (RS) has remained a formidable clinical challenge, with poor responses to standard chemotherapy. Remarkably, recent clinical studies demonstrated that 44% to 65% of patients with RS respond to PD-1 checkpoint blockade.107,108 To define the immune-mediated basis of this response, a recent study used single-cell RNA sequencing on marrow-infiltrating T cells of patients with RS who responded to and did not respond to anti-PD1 therapy. The RS marrow microenvironment was found to be enriched for cytotoxic populations, including both CD8+ effector/effector memory and cytotoxic CD4+ T cells, and expressed multiple exhaustion markers including PDCD1, LAG3, and TIGIT when compared with that of HDs. Of note, the CD8+ effector/effector memory T cells of patients with RS who did not respond showed increased expression of TOX, a master regulator of T-cell exhaustion, whereas the responders showed upregulation of the costimulatory gene CD226.109
New frontiers for single-cell analysis in CLL
The recent forays into single-cell analysis, as reviewed above, already have expanded our knowledge regarding the mechanisms of CLL disease progression and its cross talk with the immune microenvironment. These studies certainly have whetted our appetite for further extending investigations into numerous crucial areas for future study, as delineated in Figure 3.
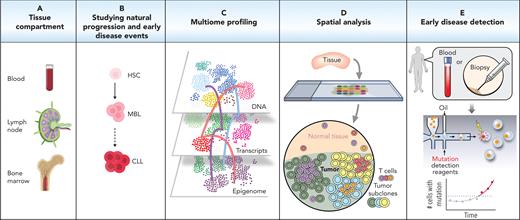
Future directions for single-cell technology in CLL. Sampling from various compartments such as the blood, lymph nodes, and bone marrow (A) and sampling from early stages of the CLL disease (B) can increase our understanding of CLL development and may aid with earlier diagnosis and treatment optimization. Additionally, using a variety of high-throughput methods such as multiome profiling (C) and spatial analysis (D) can provide an in-depth understanding of CLL and immune cell regulation and function. (E) In the future, single-cell analysis potentially could inform clinical diagnostics for early disease detection, early detection of relapse, and evaluation of the functional state and potential therapeutic vulnerabilities of the relapsed cells. HSC, hematopoietic stem cell.
Future directions for single-cell technology in CLL. Sampling from various compartments such as the blood, lymph nodes, and bone marrow (A) and sampling from early stages of the CLL disease (B) can increase our understanding of CLL development and may aid with earlier diagnosis and treatment optimization. Additionally, using a variety of high-throughput methods such as multiome profiling (C) and spatial analysis (D) can provide an in-depth understanding of CLL and immune cell regulation and function. (E) In the future, single-cell analysis potentially could inform clinical diagnostics for early disease detection, early detection of relapse, and evaluation of the functional state and potential therapeutic vulnerabilities of the relapsed cells. HSC, hematopoietic stem cell.
First, the enormous amount of molecular information that one can gain from current single-cell technologies makes it feasible to investigate cellular populations with limited tissue biopsies, including from the lymph node and bone marrow, which are common sites of disease in CLL (Figure 3A). Analysis of bulk gene expression microarrays100 already has supported the notion that the behavior of CLL and non-CLL immune cells residing in these compartments is different from that in peripheral blood. Yet to date, the vast majority of CLL studies, both bulk and single-cell analyses, have focused on circulating CLL and non-CLL immune cells because of the relative ease of obtaining blood as compared with bone marrow and lymph node specimens. Further exploration of CLL-intrinsic and immune microenvironmental features in these other disease compartments and comparison of these features with other B-cell malignancies will be certain to yield insights into the unique disease pathogenesis and clinical heterogeneity of CLL. Moreover, these discovery efforts may yield new disease biomarkers that then could become informative even when sampled from peripheral blood.
Second, defining the cellular origins of disease remains an area of high priority in the study of CLL. Single-cell analysis is uniquely capable of profiling rare cells (Figure 3B). Already, genetic and epigenetic characterizations of MBL have increased our understanding of CLL evolution with potential to facilitate earlier diagnosis,59,66 but extant questions include the order of molecular events that define this natural trajectory, as well as the precise cell of origin of CLL. Additionally, the mechanism underlying CLL progression to high-grade lymphoma remains undercharacterized. Single-cell studies of RS undoubtedly will provide mechanistic insight into the basis of CLL transformation and will facilitate in the identification of novel therapeutic targets for RS.
Third, we can envisage future studies incorporating the multilayering of genomic, transcriptomic, and epigenomic data at the single-cell level to decipher CLL heterogeneity and evolution further (Figure 3C). The integration of these complementary methods remains in developmental stages; however, the various combinations that have been tested so far each have proved to provide a better understanding of tumor progression, as well as response and resistance to therapy in CLL.58,65,67
Fourth, an exciting area of rapid development is the emergence of high-dimension spatial analysis to enable direct interrogation of the intercellular interactions and architectural organization between malignant cells and the immune microenvironment (Figure 3D). Rapid advances in these technologies have spawned diverse DNA-, RNA-, and protein-based approaches such as multiplexed error-robust fluorescence in situ hybridization,110 high-dimensional protein detection methods,111-113 and spatial barcoding.114-116 Application of these approaches will be especially relevant to the analysis of CLL samples from the bone marrow and lymph node compartments. However, a potential challenge to these studies may be the difficulties in procuring adequate tissue biopsies from patients for such studies.
Finally, we anticipate that single-cell approaches can find future clinical translation to aid CLL prognostication, therapeutic stratification, and optimization and to delineate strategies through which immunity can be harnessed for effective therapies (Figure 3E). For example, single-cell monitoring could allow early detection of rare cells bearing distinctive molecular features of the malignant clone as a harbinger of early relapse. Moreover, the profiling of the functional states of CLL cells and those of the immune microenvironment could help to select the best therapeutic combination targeting the unique tumor-intrinsic and immune microenvironmental dependencies. Certainly, as we approach the end of the beginning for the current age of single-cell technologies, we can look forward to incorporating ever more single-cell analysis in our discovery efforts into the mechanistic and therapeutic basis of CLL. Single-cell technologies also have enormous translational potential in the realm of clinical diagnostics, enabling more precise disease detection and monitoring of CLL in the future.
Acknowledgments
The authors thank Marwan Kwok for critical reading of the manuscript.
C.J.W. acknowledges support from National Institutes of Health/ National Cancer Institute grants P01 CA206978 and U10 CA180861 and from the CLL Global Research Foundation. A.N. is a T32 award recipient in the program in Molecular Immunology and Tumor Biology (5T32CA009216-41).
Authorship
Contribution: A.N. and C.J.W. conceived and wrote the manuscript.
Conflict-of-interest disclosure: C.J.W. is an equity holder of BioNtech, Inc., and receives research funding from Pharmacyclics. A.N. declares no competing financial interests.
Correspondence: Catherine J. Wu, Department of Medical Oncology, Dana-Farber Cancer Institute, Harvard Medical School, 450 Brookline Avenue, Dana 520C, Boston, MA 02215; e-mail: cwu@partners.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal