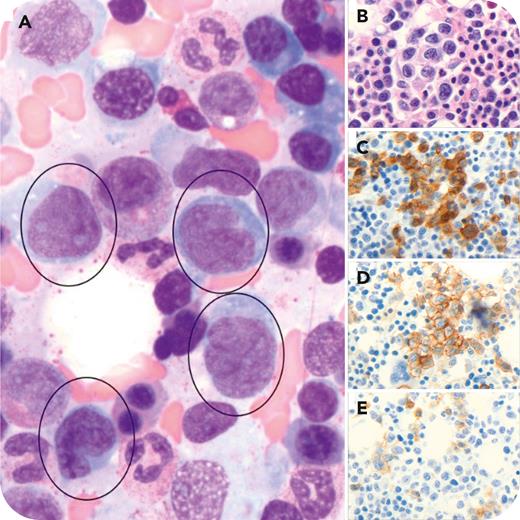
A 64 year-old woman with a 1-year history of mycosis fungoides (stage IIB, cT3N0B1M0) in treatment with ultraviolet B and bexarotene presented with cytopenias and elevated lactate dehydrogenase and alkaline phosphatase levels. A bone marrow biopsy was performed and aspirate smears showed a prominent population of large, pleomorphic cells with folded nuclear membrane, prominent nucleoli, and a moderate amount of cytoplasm, comprising about 20% of marrow cellularity (panel A, Wright-Giemsa stain; 100× objective, ×1000 original magnification). The core biopsy showed hypercellular marrow with interstitial aggregates of large cells (panel B, hematoxylin and eosin; 40× objective, ×400 original magnification) that stained positive for CD3 (panel C; 40× objective, ×400 original magnification) and CD4 (panel D; 40× objective, ×400 original magnification) and displayed loss of CD7 (panel E; 40× objective, ×400 original magnification). Plasma cells (5%-6% of cells) were polytypic. A repeat skin biopsy also showed large-cell transformation.
Involvement of bone marrow by advanced mycosis fungoides is a rare finding, with studies showing only limited examples of confirmed involvement. When confirmed, the infiltrates tend to be sparse and interstitial. The prognostic value of bone marrow involvement by advanced mycosis fungoides is unknown, but known cases presented with advanced clinical stage and subsequent death secondary to lymphoma.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal