Background: Several prognostic scores have been developed to guide management strategies in cirrhotic patients. Child-Pugh and Model of End-stage Liver Disease (MELD) are the typical scores currently used to predict outcomes in cirrhosis, however both do not include platelet count. Although platelet count may provide clues regarding severity of the disease, there is scarcity of data supporting its utility as a prognostic factor in patients with cirrhosis. Hence our study aimed to investigate the association between thrombocytopenia and development of complications as well as mortality in cirrhotic patients.
Methods: TheNational Inpatient Sample (NIS) Database was used to sample individuals with liver cirrhosis between 2016 and 2018. Baseline demographics and comorbidities were collected using ICD-10-DM codes. Patients younger than 18, those with missing data, and with history of thromboembolism were excluded. Study patients were then stratified into those with and without thrombocytopenia. Greedy propensity matching using R was performed to match the two cohorts in 1:1 ratio on age, gender, race, use of anti-thrombotic agents, smoking, and nine other comorbidities including diabetes, dyslipidemia, hypertension, morbid obesity, chronic kidney disease, end stage renal disease, chronic heart failure, history of cancer, and history of transient ischemic attack or stroke. Multivariate logistic regression model was used to analyze outcomes. P-value of <0.05 was considered statistically significant.
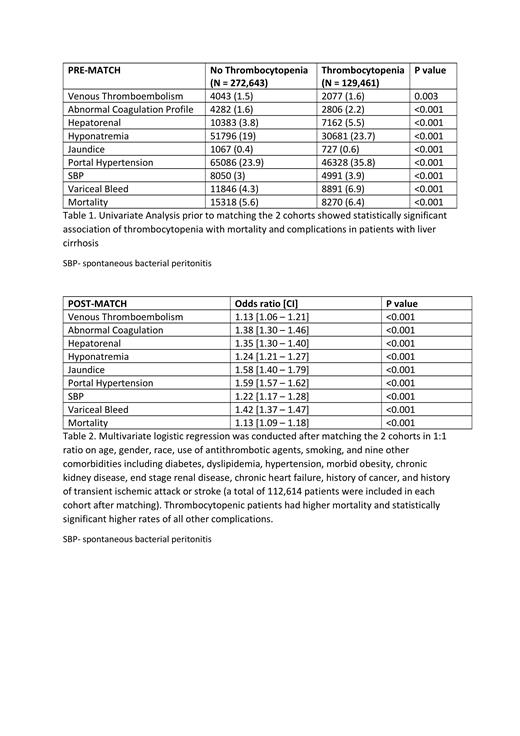
Results: Out of a total of 402,104 cirrhotic patients, 129,461 had thrombocytopenia. Thrombocytopenic patients were younger, male pre-dominant, and healthier with lower prevalence of all comorbidities and anti-thrombotic use. Thrombocytopenic patients had statistically significant higher mortality (6.4% vs 5.6%), venous thromboembolism (1.6% vs 1.5%), variceal bleeding (6.9% vs 4.3%), spontaneous bacterial peritonitis (3.9% vs 3%), portal hypertension (35.8% vs 23.9%), hepatorenal syndrome (5.5% vs 3.8%), hyponatremia (23.7% vs 19%), jaundice (0.6% vs 0.4%) and abnormal coagulation profile (2.2% vs 1.6%). Multivariate logistic regression model after matching showed similar outcomes with thrombocytopenic patients having higher mortality (OR: 1.13 [1.09 - 1.18];p<0.001) and statistically significant higher rates of all other complications.
Conclusion: Thrombocytopenia was significantly associated with higher mortality and complications in liver cirrhosis. These findings highlight the importance of considering thrombocytopenia as a poor prognostic factor when evaluating patients with liver cirrhosis. Further randomized controlled trials are needed to corroborate these findings and explore the benefit of addition of platelet count to the current prognostic scores used in clinical practice to estimate outcomes in liver cirrhosis.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal