Introduction: Relapsed/refractory T-cell acute lymphoblastic leukemia/lymphoblastic lymphoma (R/R T-ALL/LBL) is highly heterogeneous. The available salvage treatment options for relapsed patients showed remission rates of less than 50% and a 5-year overall survival (OS) rate of less than 25%. Venetoclax, a Bcl-2 inhibitor, in combination with azacitidine, has demonstrated a high remission rate in 5 patients with R/R T-ALL/LBL in our previous report. Here, we report the interim analysis of a phase 2 study (NCT05149378) for the treatment of venetoclax combined with azacitidine for R/R T-ALL/LBL.
Methods: From November 2021 to May 2023, a total of 18 R/R T-ALL/LBL patients were enrolled in the study. Among them, 11 were male and 7 were female. These patients were from seven hospitals, including the central hospital of the First Affiliated Hospital of Soochow University. All patients received salvage treatment with venetoclax (orally, 100mg on day 1, 200mg on day 2, and 400mg on days 3-21) and azacitidine(75mg/m 2/d on days 1-7, subcutaneously). Bone marrow evaluation was performed after the blood cell count recovery or within 42 days since the initiation of the treatment.
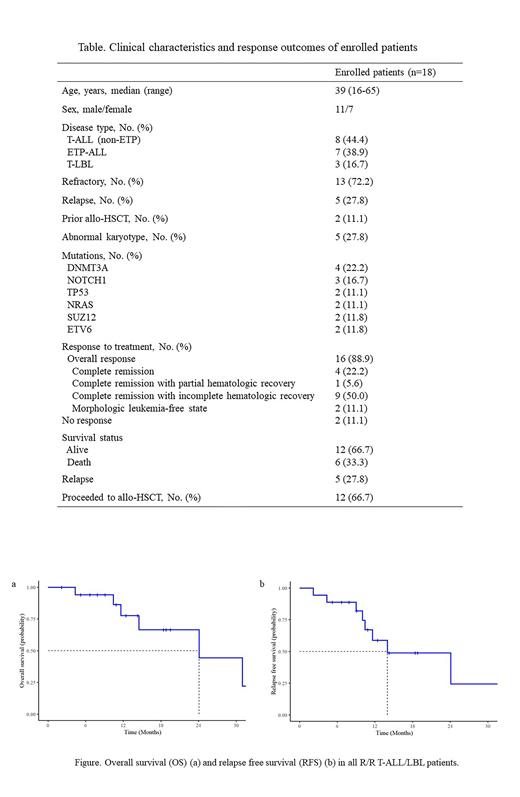
Results: Among the 18 patients enrolled, 8 were diagnosed with T-ALL, 7 with ETP-ALL, and 3 with T-LBL (Table). 5/18 patients were relapsed T-ALL/LBL, 13/18 patients were refractory to previous treatments. The median age of the patients was 39 years (range: 30-53). After 1-2 courses of venetoclax in combination with azacitidine regimen. 4 (22.2%) achieved CR, 1 patient (5.6%) achieved CRh, 9 (50.0%) patients achieved CRi and 2 (11.1%) achieved MLFS. The overall response rate was 88.9%. With a median follow-up time of 24.1 months (95% CI: 6.8-41.4), the estimated median OS was 24.1 months (95% CI: 6.8-41.4) (Figure a) and the median relapse-free survival was 14.0 (95% CI: 3.8-24.2) months (Figure b). After the treatment, 12/18 (66.7%) patients underwent allogeneic hematopoietic stem cell transplantation. Five patients experienced relapse between 6 to 19 months after the venetoclax and azacitidine treatment. Four patients died because of relapse after the regimen, two patients died because of COVID-19. Grade 3 or higher treatment-related hematologic AE included neutropenia (15/18, 83.3%), anemia (6/18, 33.3%), and thrombocytopenia (4/18, 22.2%). Treatment-related non-hematologic AE included infections (6/18, 33.3%. 4 patients developed pneumonia, 1 patient had perianal infection, 1 patient developed sepsis), elevation of ALT and AST (5/18, 27.8%), and renal function impairment (2/18, 11.1%). There was no other grade 3 or higher non-hematologic AE and no treatment-related death was observed.
Conclusion: Our results showed that venetoclax in combination with azacitidine was an effective salvage regimen for R/R T-ALL/LBL patients. The benefit of this regimen for distinct cytogenetic groups in R/R T-ALL/LBL needs to be analyzed in more cases.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal