Background: Hemato-oncological patients, and in particular patients with acute myeloid leukemia (AML) in the remission induction treatment phase frequently receive transfusion products. These products include platelet- and red blood cell- concentrates and are administered in order to prevent and treat bleeding complications and anemia. During this treatment, patients are constantly monitored by clinical laboratory tests, however, additional studies could add nuanced information about the patients' status. Different studies have shown that plasma proteins change and their patterns' characteristics could be key to illustrate the patients' healthy and/or disease status. Importantly, changes in the plasma proteome in AML patients receiving transfusion products have not yet been studied. Thus, defining protein profiles during this phase is vital to use as a point of reference prior to tracing patients' treatments and their responses.
Aim: In light of this, we aim to delineate the baseline plasma proteome in AML patients during their treatment phase.
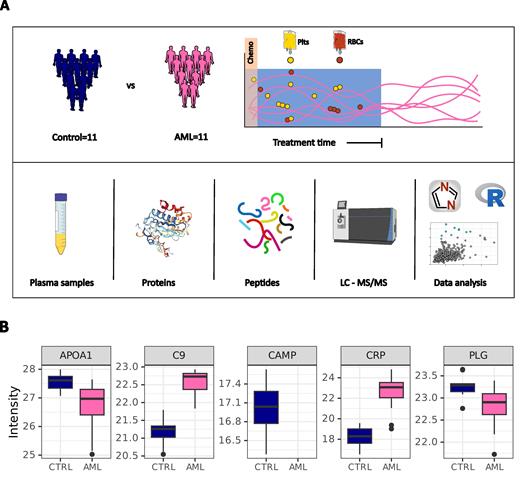
Methods: We employed unbiased mass spectrometry (MS)-based proteomics to gain insight in treatment-induced changes of the plasma proteome (Figure 1A). We included samples derived from 11 healthy donors and 11 AML patients who received chemotherapy and platelet, and red blood cell transfusions. AML patients without a previous transplant or platelet transfusion were included in this study.
Results: We identified over 400 proteins in each plasma sample and found associations between proteins and clinical laboratory data, exemplified by a high correlation between Pro-Platelet Basic Protein (PPBP) and platelet incounts (r = 0.7, p-value < 0.001). We observed 169 significantly different proteins between AML patients and healthy controls, amongst the most significant changes we captured a strong signature of inflammation with an increased abundance of proteins involved in the acute-phase response pathway (i.e. SAA1 and CRP) and a decreased abundance of proteins involved in innate immune response (i.e. DEF1 and CAMP). Interestingly, we also found an increased abundance of proteins from the complement pathway (i.e. C9 and CFHR) and decreased abundance in proteins enriching for plasma lipoprotein particle remodeling (i.e. APOA1 and PON1) (Figure 1B). Furthermore, by building correlation networks we analyzed differences in the dynamics of plasma proteins in AML patients compared to healthy controls. This analysis showed several changes in associations between proteins, including alterations in known interactions such as the gain of correlation between APOA1 and GPLD1 as well as a loss of correlation between PLG and KNG1.
Conclusion: These results highlight an imbalance in lipid metabolism and innate defense mechanisms, such as the coagulation pathway and complement system, in AML patients during their transfusion-dependent window. The plasma proteome studied in this pilot can serve as the basis to further explore changes induced in specific subgroups of patients, for example patients with and without bleeding complications. Follow up studies to analyze the changes observed here in larger cohorts are currently running (ALPHABET, trial registration NL9204) and they would be key to explore their potential association with clinical outcome in AML patients receiving transfusion products.
Figure 1.- Exploring proteome changes in AML patients during their transfusion treatment phase. A) Graphical summary of the study, and B) Proteins with contrasting dynamics when comparing AML patients in treatment phase to healthy controls. Box plots depict median with its upper and lower limits representing the first (25th) and third (75th) percentiles, respectively. Box plot whiskers extend up to the highest or lowest value within 1.5 x IQR.
Disclosures
Ypma:Janssen: Other: support for attending meetings and/or travel; Janssen: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal