Introduction: In individuals diagnosed with chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL), high-risk features are associated with an unfavorable outcome. Evidence is lacking in comparing the overall survival (OS) of a high-risk group (HRG) vs. a non-high-risk group (NHRG). This large retrospective cohort study, using data from the Flatiron Health CLL Core Registry electronic medical records (EMR), included 1,242 CLL/SLL patients treated with first-line (1L) single-agent ibrutinib. This study compared the OS of patients from the HRG (presence of deletion 17p [del(17p)], or deletion 11q [del(11q)], or unmutated immunoglobulin heavy-chain variable region gene [IGHV]) with that of patients from the NHRG (del[17p] absence, del[11q] absence, and mutated IGHV). This study also included a sensitivity analysis with an alternative high-risk definition and a subgroup analysis for Medicare patients.
Methods: The Flatiron Health EMR data includes patients with confirmed CLL/SLL diagnosis using both diagnosis code and chart abstraction. Patients aged ≥18 years were included if they initiated single-agent ibrutinib 28 days before index date (1L initiation+28 days) between 04 March 2016 and 31 January 2023. Patients were excluded if there was missing or incomplete information on their first systemic therapy or on the genetic variables of interest, or if they had other malignancies (≥2 diagnosis codes ≥30 days apart) within the prior 12 months before 1L initiation. OS (the time interval between the index date and all-cause mortality date) was assessed using Kaplan-Meier survival estimators, censoring patients without mortality information at the last activity date. COX proportional hazard model was used for pairwise comparison analysis, treating NHRG as the reference group. Potential confounders (including baseline covariates such as gender, age, race, stage, ECOG PS, comorbidities, practice type, disease type, and other biomarkers) were adjusted using inverse probability of treatment weighting (IPTW). The Medicare subgroup included patients with Medicare as the single payer or one of the multiple payers at ibrutinib initiation, which serves as a proxy for the elderly group (aged ≥65 years). A sensitivity analysis was conducted by defining HRG as those with del(17p) presence and/or unmutated IGHV and NHRG as those with del(17p) absence and mutated IGHV.
Flatiron Health mortality data were obtained from multiple sources including EMR, the U.S. Social Security Death Index, obituaries, funeral homes, which had been benchmarked against the U.S. National Death Index, demonstrating 87-92% sensitivity, 94%-99% specificity, and 96%-98% positive predictive value.
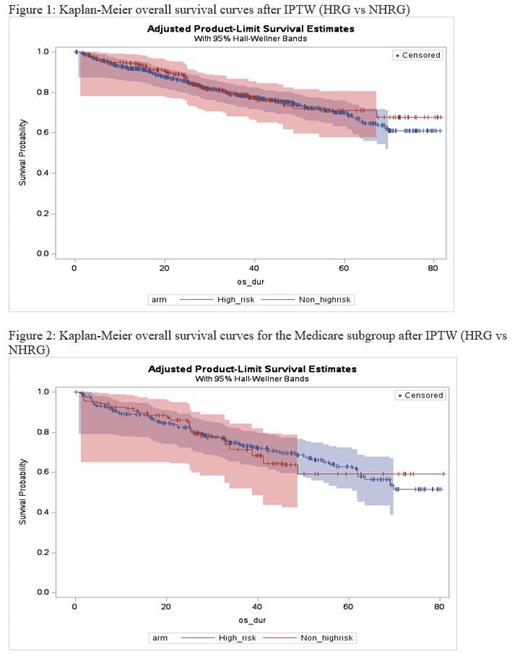
Results: Of the 1,242 patients included, 969 were from HRG and 273 from NHRG, with mean age of 70.0 vs 70.8 years. For HRG and NHRG, 36.2% vs 43.6% were female, 72.0% vs 74.7% were White, 37.5% vs 39.6% were Medicare patients (due to data limitation, 18.5% and 19.8% patients had missing data for payer type, respectively), 91.6% vs 93.8% were from the community setting, 48.8% vs 53.1% were between Rai stage 0 and II, 74% vs 70.1% had ECOG ≤ 2, 47% vs 63% had deletion 13q presence, 23.5% vs 24.2% had trisomy 12 presence, respectively. Mean (Standard Deviation) time from diagnosis to 1L initiation was 35.0 (48.0) vs 64.4 (73.2) months for HRG and NHRG. Within the HRG, 32.9%, 36.7%, and 58.7% of the patients had the presence of del(17p), del(11q), and unmutated IGHV, respectively. After applying IPTW with trimming, OS hazard ratio (HR; 95% confidence interval [CI]) was 1.09 (0.79, 1.51) and median OS was not reached for either group (Figure 1). Median follow up (interquartile range [IQR]) was 32 (17, 48) months and 31 (19, 44) months, for HRG and NHRG, respectively. The HRG sensitivity analysis showed similar results to the main analysis, with OS HR (95% CI) being 1.19 (0.86, 1.64) and median OS not reached for either group. Within the Medicare subgroup, OS HR (95% CI) was 0.98 (0.63, 1.53), and median OS was not reached for either group (Figure 2).
Conclusions: In this real-world study using a large community healthcare dataset, CLL/SLL patients with high-risk molecular-cytogenetic features (del[17p], or del[11q], or unmutated IGHV) treated with 1L ibrutinib had similar OS compared to patients without high-risk features. Importantly, similar findings were observed in the high-risk sensitivity analysis and the Medicare subgroup.
Disclosures
Allan:Lava Therapeutics: Consultancy; ADC Therapeutics SA: Consultancy; AstraZeneca: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria, Speakers Bureau; Lilly: Consultancy; BeiGene: Consultancy, Honoraria, Research Funding, Speakers Bureau; Epizyme: Consultancy; Genentech, Inc.: Consultancy, Research Funding; Janssen: Consultancy, Research Funding, Speakers Bureau; Pharmacyclics LLC: Consultancy, Speakers Bureau; TG Therapeutics, Inc: Consultancy, Research Funding; Adaptive Biotechnologies: Consultancy. Ran:Janssen Scientific Affairs, LLC: Current Employment, Current equity holder in publicly-traded company. Ding:Janssen Scientific Affairs, LLC: Current Employment, Current equity holder in publicly-traded company. He:Janssen Scientific Affairs, LLC: Current Employment, Current equity holder in publicly-traded company. Bokun:Janssen Scientific Affairs, LLC: Current Employment, Current equity holder in publicly-traded company. Qureshi:Janssen Scientific Affairs, LLC: Current Employment, Current equity holder in publicly-traded company. O'Brien:Pharmacyclics: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Lilly: Consultancy, Research Funding; Janssen: Consultancy; Johnson & Johnson: Consultancy; Regeneron: Research Funding; Beigene: Consultancy, Research Funding; Astrazeneca: Consultancy; Abbvie: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal