Introduction: Multiple sclerosis (MS) is a disabling disease that affects young adults. Treatments for MS have increased exponentially in number, efficacy and risk. Autologous hematopoietic stem cell transplantation (aHSCT) can change the natural history of the disease. To analyze if aHSCT should be done early in the course of the disease or after failing of other therapies, we have studied the long-term results of aHSCT in a cohort of persons with MS
Materials and methods: Patients with MS referred to our center for aHSCT between June 2015 and July 2023 were prospectively entered in the study. All phenotypes of MS were included (relapsing remitting, primary progressive and secondary progressive). The follow up was assessed with the patient reported EDSS score in an online form; only patients followed by three or more years were included in the analysis. ). The progression of MS was assessed by changes in the expanded disability status scale (EDSS).The response rate was analyzed for four variables: Disease-modyfing treatment (DMT) given or not before the HSCT and delay in the diagnosis and treatment: More (delayed diagnosis DD), or less (non-delayed diagnosis NDD) than 8 months after the onset of symptoms.
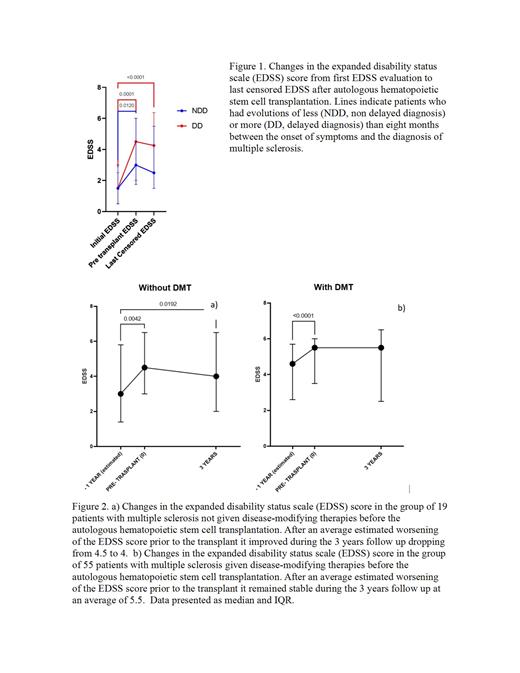
Results: 1518 subjects were prospectively enrolled. In a subset of 103 patients, detailed pre- and post-transplant evolution could be recorded. Two groups of patients were analyzed according to the time of evolution between the onset of symptoms and the definite diagnosis of MS: More than 8 months, (delayed diagnosis, DD) or less than 8 months (non-delayed diagnosis, NDD). The time elapsed between the onset of symptoms and the correct diagnosis was lower for the NDD group (1.55 vs 35.87 months, p<0.05). Both groups of patients showed a similar EDSS score at diagnosis (1.5 vs 1.5); however, the EDSS at the time of the transplant was higher in the DD group (4.5 vs 3.0, p= 0.3) and the response of the EDSS score to the transplant was significantly better for the NDD group, the last censored values for the EDSS being 2.5 vs 4.25 (p= 0.03). The two groups of patients responded to aHSCT by diminishing the EDSS, but the response was significantly better in the NDD group. On the other hand, 74 patients were followed for more than 36 months, and the subsequent analysis was done in this cohort. The response rate (RR = improvement + stabilization) at 12, 24 and 36 mo was 84%, 84% and 58% respectively for patients not receiving prior disease modifying treatments (DMT) and 72%, 90% and 67% for patients receiving DMT. In the whole group, the EDSS score dropped from a mean of 5.5 to 4.5 at 12 mo, to 5.0 at 24 mo and to 5.5 at 36 mo, after the aHSCT. The EDSS score was on average worsening in patients before the aHSCT, but the transplant stabilized the EDSS score at 3 years in patients with prior exposure to DMT, whereas in persons not given DMT, the transplant resulted in a significant decrease (p = .01) of the EDSS score. This indicates a positive response in all patients given aHSCT, but significantly better in those not exposed to DMT before the graft.
Conclusion: These data indicate that both the pre-transplant progression of the disease and the response to aHSCT were significantly worse in persons with a delayed diagnosis. An early diagnosis and an early aHSCT intervention are critical for a good prognosis, in terms of lowering and stabilizing the motor disability in MS patients given autografts. Moreover, the response to aHSCT was better for persons not exposed to immunosuppressive DMT before the transplant, thus suggesting that aHSCT should be done early in the course of the disease and probably before the treatment with DMT. Additional studies are needed to further analyze the impact of the use of DMT therapies before the aHSCT in MS, as well as the timing of the procedure.
Disclosures
Gomez-Almaguer:AMGEN: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Novartis: Honoraria; AbbVie: Consultancy, Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal