Introduction
Relapse remains the main reason for poor outcomes of patients (pts) with acute myeloid leukemia (AML). Allogeneic hematopoietic stem cell transplantation (HSCT) is the preferred post-remission treatment in pts at high risk of relapse. The presence of measurable residual disease (MRD) after intensive frontline treatment or before or after HSCT has emerged as an important predictor of relapse. Various methods are used for MRD detection, including flow cytometry and molecular assays detecting individual gene mutations (mut) such as NPM1mut. Next generation sequencing (NGS)-based assays covering multiple genes commonly mutated in AML may allow sensitive MRD detection in a broad range of pts with diverse genetic characteristics.
Methods
We established a targeted, error corrected NGS MRD assay utilizing single-molecule molecular inversion probes (smMIPs). The smMIP protocol uses a hybridization-capture approach to selectively enrich and amplify both DNA strands of 92 regions in 32 genes in a single reaction. Unique molecular identifiers (UMIs) facilitate computational correction of sequencing errors to enable reliable detection of variants ≥0.5% variant allele frequency (VAF), with the additional advantage of relatively low reagent and sequencing costs of < $100 per sample.
The smMIP assay was used to evaluate MRD status on pre-HSCT bone marrow samples from 98 AML pts who received an HSCT in first (n=83) or second (n=15) complete remission with or without count recovery. Median age at HSCT was 59 (range 20-75) years, 42% were female; 70% had de novo AML, 19% had an antecedent myeloid neoplasm and 11% had AML post cytotoxic therapy. European LeukemiaNet (ELN)-2022 risk groups at diagnosis were favorable in 11%, intermediate in 33%, adverse in 20% and unknown in 22%. All pts had received intensive induction chemotherapy. Twenty-nine percent received a myeloablative conditioning regimen (MAC), while 23% received reduced intensity conditioning (RIC) and 48% a non-myeloablative (NMA) conditioning regimen. Donors were matched related (18%), haploidentical (6%), or matched (55%) or mismatched (21%) unrelated. The median follow-up for pts alive was 34.8 months.
Results
Overall, we detected 190 variants in 71 (72%) of 98 pre-HSCT remission samples. The most commonly affected genes were DNMT3A (in 37% of pts), TET2 (21%), PPM1D (12%), IDH2 (10%) and TP53 (5%). Twenty-nine percent of pts had only variants affecting the clonal hematopoiesis-related genes DNMT3A, TET2 or ASXL1 (‘DTA‘), while 44% of patients had ≥1 variant involving a non-DTA gene. MRD-positive pts, defined as those with ≥1 non-DTA variant, had similar baseline and HSCT-related characteristics (includingage, sex, ELN risk group, de novo vs. secondary AML) compared to pts without non-DTA variants.
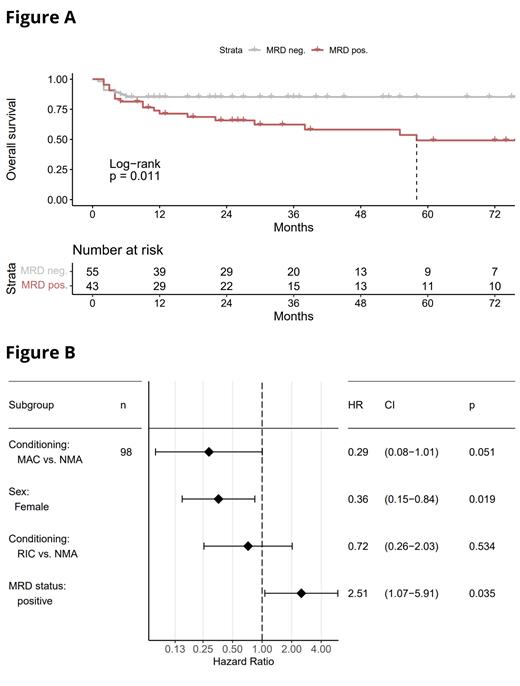
Overall survival (OS) was significantly inferior in NGS MRD-positive pts compared to those with no non-DTA variant (Figure A, 5-year OS, 49% vs. 85%, P=.011). MRD-positive pts also had a non-significant higher cumulative incidence of relapse at 5 years (46% vs. 24%, P=.14), while non-relapse mortality was similar in both groups (P=.72).
We next performed multivariable analyses, considering variables associated with OS at an univariable P<.10 (MRD status, patient sex, therapy-related AML, conditioning intensity), and using stepwise backward variable selection to identify factors significantly associated with OS (Figure B). In the final multivariable model, pre-HSCT MRD detection remained associated with inferior OS (hazard ratio 2.51; 95% confidence interval, 1.07 - 5.91; P=.035). Female sex associated with favorable OS, while myeloablative conditioning (MAC) showed a borderline significant association with superior OS. Of note, we did not detect an interaction between conditioning intensity and detection of MRD with regard to OS, i.e. the prognostic association of MRD detection was not different between pts receiving myeloablative or less-intensive conditioning. However, this analysis was limited by the small patient number.
Conclusion
Detection of MRD by targeted NGS using the smMIPs approach provides prognostic information in pts undergoing allogeneic HSCT, including those without established molecular markers such as NPM1mut. This method is applicable to a large proportion of AML pts and is cost-efficient for broad clinical use.
S.M.K. and T.H., and M.J. and K.H.M. contributed equally to this abstract.
Disclosures
Ussmann:Sanofi: Other: former travel support. Vucinic:MSD: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Sobi: Honoraria, Other: Travel/Accommodations/Expenses; Amgen: Honoraria; AstraZeneca: Honoraria; Janssen: Honoraria; Gilead/Kite: Consultancy, Honoraria; BMS/Celgene: Consultancy, Honoraria, Other: Travel/Accommodations/Expenses; Novartis: Consultancy, Honoraria; Abbvie: Honoraria. Platzbecker:Fibrogen: Research Funding; Servier: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria, Research Funding; Celgene: Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Curis: Consultancy, Research Funding; Geron: Consultancy, Research Funding; Silence Therapeutics: Consultancy, Honoraria, Research Funding; Roche: Research Funding; Merck: Research Funding; Janssen Biotech: Consultancy, Research Funding; BMS: Research Funding; BeiGene: Research Funding; MDS Foundation: Membership on an entity's Board of Directors or advisory committees; Bristol Myers Squibb: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: travel support; medical writing support, Research Funding; Amgen: Consultancy, Research Funding; Syros: Consultancy, Honoraria, Research Funding; Jazz: Consultancy, Honoraria, Research Funding; AbbVie: Consultancy. Jentzsch:Amgen: Honoraria; Novartis: Honoraria; Pfizer: Honoraria; Blueprint Medicine: Honoraria; BMS: Honoraria; JAZZ: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal