Background: Transgender and gender nonconforming (TG) youth who are at increased risk of thrombosis may be evaluated by a hematologist to discuss thromboprophylaxis prior to starting gender-affirming hormone therapy (GAHT). However, in the absence of guidelines to inform the delivery of hematologic care to such youth, variations in practice patterns may lead to suboptimal care for these individuals.
Aim: Determine hematologists' recommendations about which TG youth should be considered at higher risk of thrombosis, laboratory evaluation and medical management of such youth, and which youth should be referred for hematologic evaluation prior to starting GAHT.
Methods: From 6/2022-2/2023, we recruited hematologists caring for patients 13-22 years-old and practicing in the Midwestern U.S. for individual semi-structured interviews. Hematologists were recruited from the institutions in the footprint of the Midwest Transgender Research Collaborative. Interviews assessed demographics, practice characteristics, comfort recommending and prescribing thromboprophylaxis to TG youth, and recommendations for 1) which youth TG youth would be considered at higher risk of thrombosis; 2) laboratory evaluation; 3) recommended thromboprophylactic medication and duration; and 4) which TG youth should undergo hematologic evaluation prior to GAHT. Transcripts were analyzed using team-based framework analysis. The study was IRB approved; informed consent was obtained.
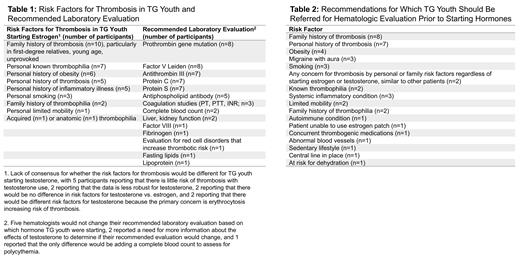
Results: Eleven hematologists from 4 academic centers participated. Mean age was 50.5 years (SD 7.2); 9 participants identified as white; 2 were Latino/a. Ten participants had provided care to TG adolescents (13-17 years-old); all 11 had provided care to TG young adults (18-22 years-old). Participants reported on average 2.8 (SD 3.3) TG adolescents and 2.5 (SD 2.9) TG young adults in their practices. Ten participants reported comfort with recommending and prescribing thromboprophylaxis to patients at higher risk of thrombosis starting estrogen for GAHT; counseling about knowledge gaps and engaging in shared decision making were important elements in the process. One participant reported preference for non-medication interventions, such as compression stockings and using lower doses or transdermal formulations of estrogen. There was less consensus around attitudes toward prophylaxis for youth starting testosterone for GAHT: 4 participants reported lower likelihood of recommending thromboprophylaxis due to low risk of thrombosis with testosterone use; 3 participants discussed risk of erythrocytosis/polycythemia due to testosterone use (although there was no consensus on whether prophylaxis would be recommended); 3 participants reported comfort prescribing prophylaxis to youth starting testosterone; and 2 participants reported insufficient knowledge about the thrombotic risks of testosterone. Hematologists reported various factors that would lead to TG youth being considered high risk, as well as recommended lab testing (Table 1). If prophylaxis is needed, 10 participants would recommend a direct anticoagulant, while 1 would recommend aspirin. Five participants anticipated that long term prophylaxis would be needed for the duration of GAHT, while 6 reported duration would be individualized. Ten participants would not recommend against estrogen due to thrombosis risk, emphasizing the importance of gender care and the role of the hematologist in making GAHT as safe as possible. No participant would recommend against testosterone. Participants offered recommendations for which TG youth should be evaluated by a hematologist prior to starting GAHT (Table 2).
Conclusion: Overall, hematologists voiced comfort with recommending and prescribing thromboprophylaxis to TG youth at higher risk of thrombosis starting estrogen. However, there was lack of consensus about evaluation of youth at higher risk of thrombosis starting testosterone and whether mitigation of risk would be needed. Developing guidance for gender care teams for which youth should be considered at higher risk of thrombosis and referred for hematologic evaluation would help optimize the safe delivery of gender-affirming hormone care. Additional data and guidance about the thrombosis risks associated with GAHT is needed to better inform hematologic care.
Funding: NIH R01HL161153; Cincinnati Children's Hospital Medical Center Gap Funding
Disclosures
Mullins:Takeda: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal