Sickle cell disease (SCD) is an inherited hemoglobin (Hb) disorder which leads to significant morbidity and early mortality. Hematopoietic cell transplantation (HCT) is the only curative treatment with long-term outcome data, demonstrating excellent symptom-free survival particularly when a matched related donor (MRD) is available. Most MRD have sickle cell trait (Hb AS), but trait donor HCT is considered acceptable by the FDA and without negative impact. Further, initial gene addition and editing approaches for SCD have resulted in a trait-like status with benefit. Sickle trait, however, is associated with complications such as papillary necrosis, bacteriuria, splenic infarction, and exercise-induced death. The primary aim of this study was to compare long-term outcomes following MRD HCT for SCD based on donor Hb genotype, to objectively describe any impact on outcomes.
Retrospective data was available for this analysis on 182 SCD patients ≥1 year post MRD HCT at 10 participating Sickle Transplant Advocacy and Research (STAR) Alliance centers. Summary statistics were presented as mean (standard deviation) for continuous variables and count (%) for categorical variables. Comparisons were made between Hb AA and Hb AS donor groups using both parametric and non-parametric tests for continuous variables and Chi-square test/exact test for categorical variables, with p-value <0.05 set as significant.
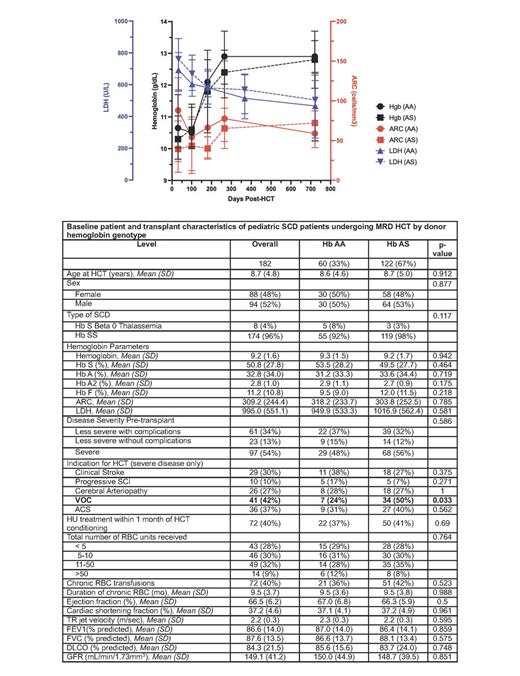
Amongst 182 patients undergoing MRD HCT, 67% (n=122) had a Hb AS donor ( Table). In the overall cohort, median age at HCT was 8.7 (4.8) years and most patients had HbSS (n=174; 96%) with a severe clinical phenotype (n=97; 54%). HCT was performed using bone marrow (n=166; 92%) with myeloablative conditioning (n=156; 86%) in the majority. Patients with a severe disease phenotype and Hb AS donor were significantly more likely to have recurrent vaso-occlusive pain crises as an indication for HCT (p=0.033), otherwise there were no differences in baseline patient or HCT characteristics between cohorts. With mean post-HCT follow up of 4.5 (3.9) and 5.1 (4.1) years in Hb AA and Hb AS donor cohorts (p=0.145), no significant differences were seen in recipient outcomes including time to neutrophil and platelet engraftment, number of or time to last platelet transfusion, myeloid or unsorted % donor chimerism, number with acute (day 100) or chronic GVHD (1 year), or time to discontinue immunosuppression (data not shown). Disease recurrence and need for 2 nd HCT were rare in both cohorts (AA: 2 [3%] and 2 [3%]; AS: 3 [3%] and 4 [3%]; p=0.665 and 1.0, respectively). Two (3%) and 5 (4%) patients died in the AA and AS cohorts, respectively (p=1.0). Aside from a statistically (but not clinically) significant difference in Hb at day 30 (p=0.044), no difference was seen in longitudinal Hb or markers of hemolysis (LDH and ARC; Figure). No significant difference was seen in median number of RBC units transfused (AA: 4.0 [2.0-6.0]; AS: 3.0 [2.0-6.0]; p=0.454) or days to last transfusion (AA: 23.0 [14.0-77.0]; AS: 22.0 [13.0-75.0]; p=0.86). SCD complications were rare post-HCT, with no difference seen between cohorts in number (%) with VOC (AA: 1 [2%; had 2 separate VOC events]; AS: 3 [3%]; p=1.0), ACS (none reported), chronic pain (AA: 0 [0%]; AS: 1 [<1%]; p=1.0), or other SCD-related complications (AA: 2 [3%]; AS: 9 [7%; had 11 separate other events]; p=0.456). Stroke occurred in a significantly higher proportion with an AA versus AS donor (5 [8%] and 2 [2%], respectively; p=0.04). No significant differences were seen in longitudinal (1 and 2 years and at last follow up) post-HCT cardiac (EF, SF, TRJ velocity), pulmonary (FEV1, FVC, DLCO), or renal (GFR) function between cohorts (data not shown).
Our results indicate that in MRD HCT for SCD, AS and AA donors yield comparable long-term outcomes. In this retrospective and registry-based study design, detailed analyses did not show differences between the two cohorts at baseline or at any timepoint post-HCT. While there were some outcome differences between the cohorts, they were either not clinically significant or did not have a scientific rationale, and thus were likely due to chance alone (denoted by bolding in Table). Given the young age of our cohort at HCT and thus a smaller proportion with SCD-related organ dysfunction, our results may not be applicable to an older cohort with significant organ dysfunction which will require a separate analysis.
Disclosures
Stenger:bluebird bio, Inc.: Research Funding. John:bluebird bio: Consultancy, Membership on an entity's Board of Directors or advisory committees; vertex: Membership on an entity's Board of Directors or advisory committees. Guilcher:Bristol Myers Squibb: Research Funding; bluebird bio, Inc.: Research Funding. Kasow:Aruvant: Consultancy, Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal