Background: Factor XI(FXI) deficiency is a rare and relatively mild bleeding disorder. To date, data for China is limited. Our study aimed to investigate the clinical phenotype, F11 genotype and management of individuals diagnosed with FXI deficiency from throughout China.
Methods: The study retrospectively analyzed patients with FXI activity (FXI:C) <50% registered from the National Hemophilia Registration System. The study collected patient characteristics, F11 gene mutations, clinical history, bleeding events, and treatment strategy by telephone follow-up.
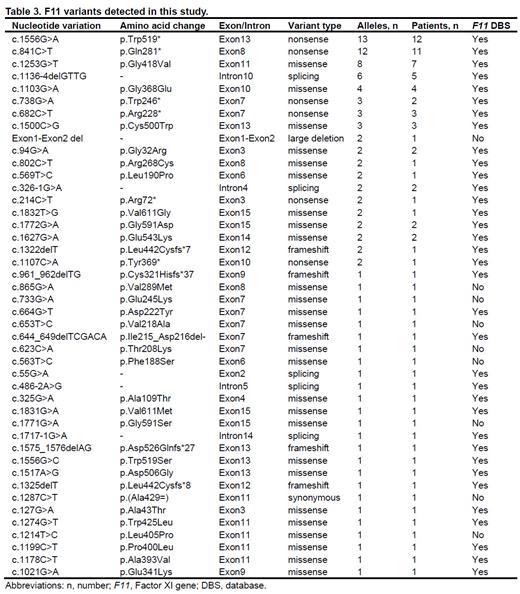
RESULTS: The study included 234 patients throughout 27 provincial districts registered in 38 Chinese hemophilia treatment centers. Among these patients, 192 (82.1%) had severe FXI deficiency (FXI:C <15%), and 42 (17.9%) had non-severe FXI deficiency (15%≤FXI:C<50%). The median age was 30 (1-87) years at diagnosis. There were 19 patients (8.1%) who reported a family history of bleeding. Five patients (2.1%) reported having consanguineous marriages in their families. There were 57 patients (24.4%) had their F11 gene tested. We detected 44 kinds of variants on 99 alleles, including nine that have never been reported to the F11 database. The most frequent variants were missense (44, 44.4%) and nonsense mutations (35, 35.4%). Among the genotyped subjects, F11 mutations were homozygous in 12 (21.0%), compound heterozygous in 29 (50.9%), and heterozygous in 16 (28.1%) patients. The FXI:C among patients with homozygous/compound heterozygous mutations was significantly lower than among patients with heterozygous mutations (2.1±2.3% vs. 14.8±12.9%, P<0.001). In total, 91 (38.9%) reported bleeding symptoms to varying degrees. Among these patients, 79 (33.8%) experienced spontaneous bleeding, with menorrhagia, epistaxis, and dermatorrhagia being the most prevalent manifestations. Twenty-one (26.6%) patients were administered on-demand replacement therapy. There were 129 patients underwent 220 invasive procedures with a total of 22 bleeding episode. The risk of bleeding was found to be significantly higher when sites with high fibrinolysis were involved, as compared to sites without fibrinolysis (Chi2=3.976, P=0.046). The prophylactic replacement treatment was administered to 50 cases (22.8%), and three bleeding events occurred, compared to 19 bleeding events in the 170 cases without prophylaxis. It was observed that prophylaxis did not reduce bleeding events (Chi2=1.150, P=0.283). A total of 83 deliveries were recorded in 58 female patients, and four bleeding events occurred. The blood group-O is a risk factor for bleeding [odds ratio (OR)=2.429, 95% confidence interval (CI) 1.139-5.182].
Conclusion: Most patients had no or mild bleeding symptoms. Most F11 variants were missense. The FXI:C among patients with homozygous/compound heterozygous mutations was significantly lower than among patients with heterozygous mutations. The risk of bleeding was higher when procedure sites with high fibrinolysis were involved. Prophylactic repalcement treatment could not reduce the risk of hemorrhages after invasive procedure. There is increased risk of bleeding in patients with blood group-O.
Table 1
Table 2
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal