Introduction: Heparin-Induced Thrombocytopenia (HIT) is a prothrombotic reaction to heparin exposure caused by antibodies directed towards heparin-platelet protein platelet factor 4 complexes. This thrombocytopenia is associated with and can lead to fatal venous and arterial thrombosis. This study aims to compare outcomes and assess the association of autoimmune diseases with HIT.
Methods: A query of the National Inpatient Sample (2016-2020) was performed for index admissions with a principal diagnosis of HIT and concurrent autoimmune diseases using ICD 10 codes. Patient demographics and outcomes were identified. Univariate analysis with t-test or chi-squared was performed where appropriate. A multivariate regression analysis was used to generate adjusted odds ratios (AOR), adjusting for age, race, sex, and Charlson Comorbidity Index (CCI) score. The P-value significance was set at <0.05. All analysis was performed in STATA MP version 14.2.
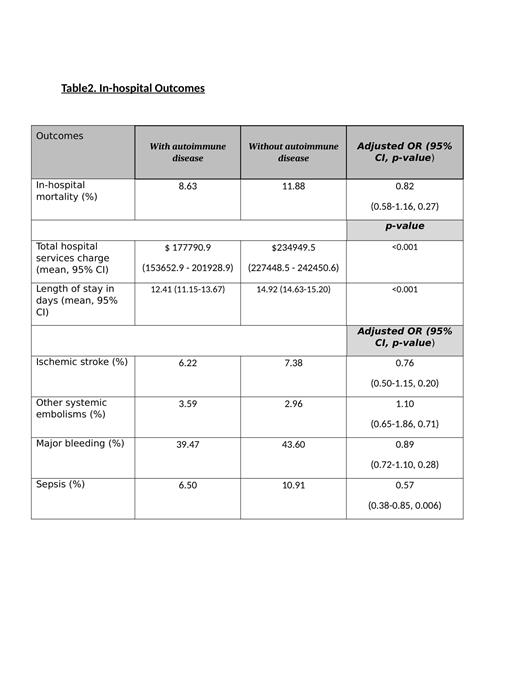
Results: A total of 72,935 patients with HIT met the inclusion criteria, of which, 2.88% had an underlying autoimmune disease. Those with auto-immune disease had a greater proportion of Caucasians, females, and younger patients. While there were no statistically significant differences in mortality, embolic, or bleeding events, patients with autoimmune disease were 43% less likely to become septic (AOR 0.57, p-value 0.006). Additionally, patients with autoimmune diseases had a lower mean hospital services charge and length of stay (p<0.001).
Conclusion: Patients with HIT and autoimmune disease showed better outcomes in terms of sepsis, mean length of stay, and hospital services charge without any significant difference in embolic or bleeding outcomes. Underlying autoimmune disease likely does not confer any additional risk to HIT hospitalizations. This might be speculated to be due to the different underlying pathology driving HIT or accompanying immunosuppressants treatment in autoimmune diseases hindering the aggressiveness of immune response.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal