Acute abdominal abnormalities are relatively uncommon during the treatment of acute leukaemia but, historically, have been associated with high mortality rates (Hawkins JA, Mower WR, Nelson EW. Acute abdominal conditions in patients with leukaemia. Am J Surgery 1985;150:739-742). Given the improvement in diagnostic and supportive measures for patients with acute myeloid leukaemia (AML) over time, we aimed to determine the rate and outcomes of acute abdominal and pelvic complications in a cohort of AML patients at our hospital.
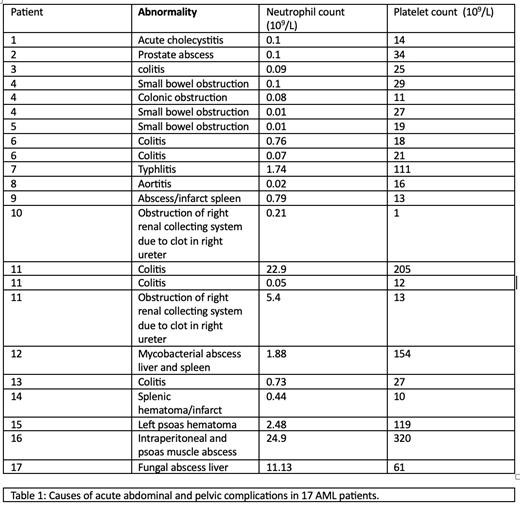
We retrospectively reviewed the medical records, radiology reports and laboratory test results of 70 consecutive newly diagnosed, non-promyelocytic AML patients undergoing intensive induction chemotherapy between January 2012 and December 2019. Seventeen patients developed 22 episodes of acute abdominal or pelvic pathology and were investigated by radiology (abdominal X ray, CT scan and/or MRI). Table 1 summarises the underlying causes for these complications, as well as neutrophil count and platelet count at time of presentation. Colitis was the most common complication, occurring 6 times. The neutrophil count was <1x10 9/L in 15 of the 22 episodes. Platelet count <20x10 9/L occurred in 8 of the episodes, including the 2 cases of ureteric obstruction by clot. All complications resolved completely with conservative management, except for 1 patient who required surgical drainage of an intraperitoneal and psoas muscle abscess in addition to intravenous broad spectrum antibiotics.
In conclusion, acute abdominal and pelvic complications were relatively rare in our cohort of patients. All but 1 of these episodes resolved with conservative management alone. These results suggest that, with current diagnostic and therapeutic measures, the prognosis for non-promyelocytic AML patients who develop such complications is favorable.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal