Sickle Cell Anemia (SCA) causes significant acute complications, chronic complications, and premature mortality. The foundational treatment for SCA is hydroxyurea (HU) which reduces acute and chronic complications. Several barriers prevent patient HU adherence and thus treatment benefit.
We performed a cross-sectional study of 206 pediatric, adolescent, and young adult (AYA) patients with HgbSS or HgbS-beta-thalassemia-zero in the United State Military Health System who were prescribed HU to evaluate for to factors associated with HU adherence. These patients have access to military or civilian pediatric hematology care at no or low cost.
We categorised patient's adherence dichotomously according to the American Society of Hematology quality metric for HU adherence. The adherence group, 26% of the study population, had a younger mean age, 11.7 versus 14.9 (p = 0.0003), and was more likely to receive hematology care in the MHS.
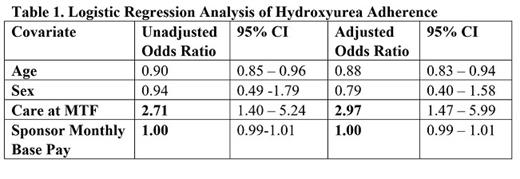
Logistic regression analysis of HU adherence, adjusted for age and gender demonstrated the patients receiving pediatric hematology care at a military healthcare facility had 2.96 (1.47-5.99, 95% CI) the odds of adherence compared to patients receiving pediatric hematology care at civilian healthcare facilities. The monthly base pay of the patient's sponsor, a strong indicator of socioeconomic status was not associated with HU adherence odds ratio 1.00 (0.99-1.01, 95% CI).
Among Pediatric and AYA patients with SCA in the MHS: HU adherence appears equitable throughout the range of sponsor rank; and hematology care at military facilities is associated with increased HU adherence.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal