In this issue of Blood, Chiba et al reveal the molecular mechanisms that control the expression of programmed cell death ligand 1 (PD-L1) in adult T-cell leukemia/lymphoma (ATLL) and propose an original therapeutic approach to treat this highly aggressive T-cell malignancy.1
ATLL is an aggressive mature T-cell lymphoid malignancy caused by human T-cell leukemia virus type 1 (HTLV-1) infection. The prognosis is very poor, especially in aggressive subtypes, which represent the majority of the cases at diagnosis, with an overall survival (OS) of <1 year.2 In these subtypes, the standard of care is polychemotherapy (ie, CHOP-like regimen [cyclophosphamide, hydroxydaunorubicin, vincristine (Oncovin), prednisone] or the LSG-15 protocol in Japan that consists of a sequential combination of chemotherapies: VCAP [vincristine, cyclophosphamide, doxorubicin, prednisone], AMP [doxorubicin, ranimustine, prednisone], and VCEP [vindesine, etoposide, carboplatin, prednisone]) followed by allogeneic hematopoietic stem cell transplantation (alloSCT), when feasible. Apart from alloSCT, which proved to cure some patients and improve ATLL outcome,3 no significant improvement in OS has been observed since the original work by Shimoyama describing different ATLL subtypes in 1991.2 Notably, targeted therapies, such as “antiviral therapy” with the combination of zidovudine-interferon and anti–C-C chemokine receptor 4 (CCR-4) antibody (mogamulizumab), have not been able to improve significantly the outcome of ATLL.4,5 One of the main drawbacks of ATLL treatment is the intrinsic chemoresistance of the disease, with around 40% of cases presenting with primary chemoresistance.5
In the past decade, the molecular understanding of ATLL has progressed. The genetic and epigenetic landscape of ATLL is now better characterized, with the identification of at least 5 key recurrent pathways, including the T-cell receptor/NF-κB pathway (∼75% of cases), T-cell trafficking (∼45%), immunoescape (∼30%), cell-cycle regulation and tumor suppression (∼25%), and Janus kinase–signal transducer and activator of transcription (JAK-STAT) signaling (∼20%).6,7 Interestingly, these alterations are not restricted to HTLV-1–related lymphomagenesis, but are shared with other peripheral B- and T-cell lymphomas. Furthermore, ethnic background does not seem to affect the genomic landscape of ATLL. Similarly, thanks to high-throughput genomic sequencing techniques, the understanding of the role of the oncovirus in lymphomagenesis has improved.8
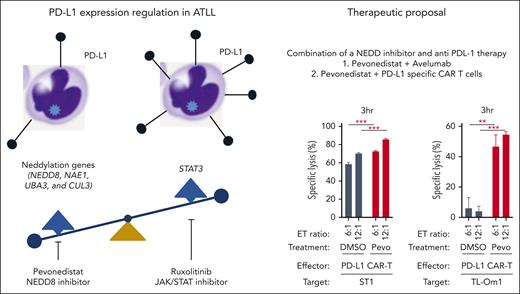
In their study, Chiba and colleagues used an unbiased approach based on CRISPR whole genome technology to elegantly identify molecular pathways regulating PD-L1 expression (see figure). They demonstrated that STAT3 is a positive regulator of PD-L1 expression and identified several neddylation pathway genes (NEDD8, NAE1, UBA3, and CUL3) as negative regulators of PD-L1 expression. In vitro studies using a pharmacological inhibitor of JAK-STAT (ruxolitinib) or neddylation (pevonedistat) provided further support for these observations. Moreover, increased PD-L1 expression by the neddylation inhibitor pevonedistat alone strongly upregulated PD-L1 expression and had a cytotoxic effect on ATLL cells in vitro. The authors pursued an interesting approach by combining pevonedistat (to increase PD-L1 expression) with an anti–PD-L1 monoclonal antibody (avelumab) or with PD-L1 specific chimeric antigen receptor T cells to target ATLL cell lines. Finally, they demonstrated an increased in vitro cytotoxic effect when using combination therapy.
Identification of molecular pathway and pharmacological compounds that regulate PD-L1 expression in ATLL and proposal for a novel combined therapy. PD-L1, programmed cell death ligand 1; NEDD8, neural precursor cell expressed, developmentally downregulated 8; NAE1, NEDD8-activating enzyme; UBA3, ubiquitin-like modifier activating enzyme 3; CUL3, cullin 3; STAT3, signal transducer and activator of transcription 3. The graphs are reproduced from Figure 7G-H in the article by Chiba et al that begins on page 1379.
Identification of molecular pathway and pharmacological compounds that regulate PD-L1 expression in ATLL and proposal for a novel combined therapy. PD-L1, programmed cell death ligand 1; NEDD8, neural precursor cell expressed, developmentally downregulated 8; NAE1, NEDD8-activating enzyme; UBA3, ubiquitin-like modifier activating enzyme 3; CUL3, cullin 3; STAT3, signal transducer and activator of transcription 3. The graphs are reproduced from Figure 7G-H in the article by Chiba et al that begins on page 1379.
Chiba et al address a gap in our understanding of the biology of ATLL as well as the urgent clinical need for novel therapeutic approaches. Their observations are applicable both in the context of wild-type PD-L1 and of somatic variants in the 3'-untranslated regions of PD-L1 frequently observed in ATLL (∼30% of cases).9 However, from a clinical point of view, the major point of concern is that using anti–PD-L1/anti–PD-1 targeted therapy could actually stimulate growth of specific clones. Indeed, therapeutic approaches using anti–PD-1 antibodies as checkpoint inhibitors have already been reported and have led to an unexpected outcome: rapid progression in several cases of indolent ATLL.10 Therefore, a better understanding of the biology of PD-L1/PD-1 in ATLL is essential to allow for safe use of a new class of potent drugs (immune checkpoint inhibitors), which are potentially dangerous in the context of ATLL.
In conclusion, despite the absence of an animal model to reinforce these novel results, the findings are of interest for scientists investigating ATLL molecular and cell biology, for clinicians who treat patients with ATLL, and more broadly for biologists interested in the regulation of immune checkpoint molecule expression.
Conflict-of-interest disclosure: The author declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal