To the Editor:
Human T-lymphotropic virus type I (HTLV-I) is associated with a number of human diseases, most notably adult T-cell leukemia (ATL) and a chronic progressive neurologic disease that resembles multiple sclerosis (MS) termed HTLV-I–associated myelopathy/tropical spastic paraparesis (HAM/TSP).1-3 How infection with HTLV-I results in neurologic disease remains elusive, but may be related to latent viral infection associated with an immunopathogenic mechanism.3 HAM/TSP patients develop an activated immune response characterized by spontaneous lymphoproliferation of peripheral blood lymphocytes4 and elevated levels of CD8+, HLA class I restricted cytotoxic T-cell (CTL) specific for immunodominant HTLV-I peptides.5 What drives this activated immune response and how it is related to the immunopathogenesis of this disease is unknown.
A significant factor in the ability of neurotropic retroviruses to cause disease is persistent viral replication while avoiding immunologic elimination.6-9 In HAM/TSP, HTLV-I is present in peripheral CD4+ T cells10; however, the localization of HTLV-I to specific immune organs has not been identified. Because the bone marrow (BM) is critical for the development of autoimmune disease11 and latent viral infection of immune organs is critical in the development of retroviral associated human diseases,8 9 we hypothesized that the BM in patients with HTLV-I–associated neurologic disease may be a source of retroviral latency. Therefore, polymerase chain reaction/in situ hybridization (PCR/ISH) and ISH12 were used to define the distribution of HTLV-I in BM of HAM/TSP patients.
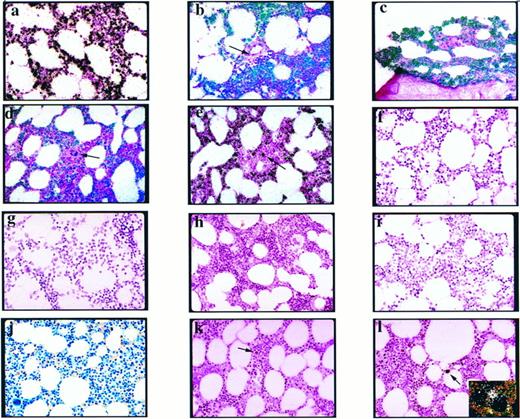
Previously, we showed that PCR/ISH of HTLV-I-tax DNA has a sensitivity of 1 to 2 copies of target DNA per cell and there was no leakage of PCR product from infected target cells to adjacent uninfected cells to produce a false-positive signal.12 Initial experiments were performed on BM from a HAM/TSP autopsy (Fig 1a) and replicated in BM biopsy samples from two additional patients (Fig 1b and c). BM morphology was normal in all cases (Fig 1j). PCR/ISH of HTLV-I-tax DNA showed extensive infection of BM cells in all three HAM/TSP samples (Fig 1a-c). Although the phenotype of these HTLV-I–infected BM cells is not yet defined immunocytochemically, there were cells without HTLV-I-tax DNA signal, most notably megakaryocytes (Fig 1d), mature red blood cells (Fig 1e), and endothelial cells surrounding blood vessels (Fig 1b). Only a rare cell in these samples was positive for HTLV-I-tax RNA by ISH (Fig 1l). The observation of cells infected with viral DNA that do not express viral RNA is consistent with the concept of viral latency.6 8 In comparison to the extensive HTLV-I infection of HAM/TSP BM (Fig 1a-c), PCR/ISH and ISH of spleen and lymph node from the HAM/TSP autopsy case showed a rare HTLV-I–infected cell (data not shown).
Autoradiograms of BM biopsy specimens from HAM/TSP patients and normal, uninfected controls following PCR/ISH and ISH (hematoxylin and eosin counterstain, which stains nuclei purple and cytoplasm pink) (all photomicrographs are original magnification ×400). (a) PCR/ISH of HTLV-I-tax DNA in a BM autopsy specimen from patient 1. Extensive HTLV-I-tax DNA signal (brightfield microscopy, silver grains appear black). (b) PCR/ISH of HTLV-I-tax DNA in a BM biopsy specimen from patient 2. Extensive HTLV-I-tax DNA signal present (combined epiflourescence and transillumination, silver grains appear green above purple, hematoxylin-stained cells); however, there is minimal signal in endothelial cells surrounding blood vessels (arrow). (c) PCR/ISH of HTLV-I-tax DNA in a BM biopsy specimen from patient 3. Extensive HTLV-I-tax DNA signal present. (d) PCR/ISH of HTLV-I-tax DNA from an HAM/TSP patient, showing minimal signal around a megakaryocyte (arrow). (e) PCR/ISH of HTLV-I-tax DNA from an HAM/TSP patient, showing minimal signal of mature red blood cells surrounding a positive cell (arrow). (f ) PCR/ISH using HTLV-I-tax DNA specific primers plus Taq polymerase, after detection of the HTLV-I-tax–amplified product with a heterologous probe. There is no positive signal. (g) PCR/ISH of HTLV-I-tax DNA in a BM biopsy specimen of an uninfected, normal patient. There are no positive cells. (h and i) PCR/ISH of HTLV-I-tax DNA of the BM biopsy of patient 1, excluding Taq polymerase (h) or HTLV-I-tax–specific primers (i) from the PCR cocktail, and detection of the amplified product with the HTLV-I-tax probe. No positive cells. (j) Modified Giemsa (Lennert) stain of a representative field of BM biopsy specimen from an HAM/TSP patient showing normal hematologic morphology. (k) ISH for HTLV-I-tax DNA. There are no positive cells and no nonspecific probe binding to eosinophils (arrow). (l) ISH for HTLV-I-tax RNA in a BM biopsy specimen of an HAM/TSP patient. A single positive cell (arrow) is present. (Inset) Darkfield microscopy of same cell showing white silver grains above cell nucleus.
Autoradiograms of BM biopsy specimens from HAM/TSP patients and normal, uninfected controls following PCR/ISH and ISH (hematoxylin and eosin counterstain, which stains nuclei purple and cytoplasm pink) (all photomicrographs are original magnification ×400). (a) PCR/ISH of HTLV-I-tax DNA in a BM autopsy specimen from patient 1. Extensive HTLV-I-tax DNA signal (brightfield microscopy, silver grains appear black). (b) PCR/ISH of HTLV-I-tax DNA in a BM biopsy specimen from patient 2. Extensive HTLV-I-tax DNA signal present (combined epiflourescence and transillumination, silver grains appear green above purple, hematoxylin-stained cells); however, there is minimal signal in endothelial cells surrounding blood vessels (arrow). (c) PCR/ISH of HTLV-I-tax DNA in a BM biopsy specimen from patient 3. Extensive HTLV-I-tax DNA signal present. (d) PCR/ISH of HTLV-I-tax DNA from an HAM/TSP patient, showing minimal signal around a megakaryocyte (arrow). (e) PCR/ISH of HTLV-I-tax DNA from an HAM/TSP patient, showing minimal signal of mature red blood cells surrounding a positive cell (arrow). (f ) PCR/ISH using HTLV-I-tax DNA specific primers plus Taq polymerase, after detection of the HTLV-I-tax–amplified product with a heterologous probe. There is no positive signal. (g) PCR/ISH of HTLV-I-tax DNA in a BM biopsy specimen of an uninfected, normal patient. There are no positive cells. (h and i) PCR/ISH of HTLV-I-tax DNA of the BM biopsy of patient 1, excluding Taq polymerase (h) or HTLV-I-tax–specific primers (i) from the PCR cocktail, and detection of the amplified product with the HTLV-I-tax probe. No positive cells. (j) Modified Giemsa (Lennert) stain of a representative field of BM biopsy specimen from an HAM/TSP patient showing normal hematologic morphology. (k) ISH for HTLV-I-tax DNA. There are no positive cells and no nonspecific probe binding to eosinophils (arrow). (l) ISH for HTLV-I-tax RNA in a BM biopsy specimen of an HAM/TSP patient. A single positive cell (arrow) is present. (Inset) Darkfield microscopy of same cell showing white silver grains above cell nucleus.
Controls used to substantiate the specificity of the HTLV-I-tax signal included the following: (1) no detectable signal in BM from an uninfected individual following PCR/ISH or ISH (Fig 1g); (2) no detectable signal in BM of HAM/TSP patients if either Taq polymerase (Fig 1h) or HTLV-I-tax–specific primers (Fig 1i) were eliminated from the PCR cocktail; (3) no detectable signal in BM of HAM/TSP patients if a heterologous (“non-sense”) probe was used during ISH after PCR (with PCR cocktail containing all reagents) (Fig 1f ); (4) an internal tissue control, in which not every cell type was positive in BM (as described above); and (5) no evidence of nonspecific binding of eosinophils or other granulocytes with either the sense (Fig 1k) or anti-sense (Fig 1l) HTLV-I-tax probe. Also, the presence of HTLV-I-tax and -pol proviral DNA was confirmed by solution phase PCR followed by Southern hybridization (data not shown).
These results show that BM may be an important reservoir of HTLV-I in patients with HTLV-I–associated neurologic disease as detected by PCR/ISH of HTLV-I-tax proviral DNA. Although the phenotype of which cell(s) within the BM of HAM/TSP patients contain HTLV-I is under study, retroviral infection of BM may be important in the pathogenesis of this chronic neurotropic retroviral disease and other disorders of suspected viral etiology and/or autoimmune involvement. Extensive latent retroviral infection of BM in these patients could be a source of virus that drive the heightened HTLV-I–specific immune responses thought to be associated with the pathogenesis of this disease. It remains to be determined if BM from asymptomatic carriers or other patients with HTLV-I–associated disorders also contain high levels of latent retrovirus in BM. As we have shown for latent retroviral infection of BM in HAM/TSP patients, it would be useful to study the BM of other patients with chronic progressive disease with autoimmune components (like MS) for the presence of known or potentially novel human retroviruses.
ACKNOWLEDGMENT
We thank W. Biddison, R. Gress, and H. McFarland for critical review of this study and helpful suggestions, and J. Eberwine for his contribution to these experiments. M.C.L. is a postdoctoral fellow of the Multiple Sclerosis Society. R.J.F. is a Howard Hughes Medical Institute-N.I.H. Medical Student Scholar.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal